REFLECTION ARTICLE
SYSTEMIC ARTERIAL HYPERTENSION AS A DETERMINING FACTOR IN TRIGGERING CEREBRAL HEMORRHAGES: A REFLECTIVE ANALYSIS
LA HIPERTENSIÓN ARTERIAL SISTÉMICA COMO FACTOR DETERMINANTE EN EL DESENCADENAMIENTO DE HEMORRAGIAS ENCEFÁLICAS: UN ANÁLISIS REFLEXIVO
HIPERTENSÃO ARTERIAL SISTÊMICA COMO FATOR DETERMINANTE PARA DESENCADEAMENTO DE HEMORRAGIAS ENCEFÁLICAS: UMA ANÁLISE REFLEXIVA
https://doi.org/10.31011/reaid-2026-v.100-n.1-art.2538
João Victor Bassan do Nascimento1
Francis Marcos Bedin2
Rafael Schimitt da Rosa3
Daniela Lima de Camargo4
Fábila Fernanda dos Passos da Rosa5
1Centro Universitário da Fundação Educacional de Brusque - UNIFEBE. Balneário Camboriú - SC, Brazil. ORCID: https://orcid.org/0009-0009-9731-3540. e-mail: joao.donascimento@unifebe.edubr
2Centro Universitário da Fundação Educacional de Brusque - UNIFEBE. Brusque-SC, Brazil. ORCID: https://orcid.org/0009-0005-1703-4068. e-mail: francis.bedin@unifebe.edu.br
3Centro Universitário da Fundação Educacional de Brusque - UNIFEBE. Balneário Camboriú - SC, Brazil.
ORCID: https://orcid.org/0009-0000-9681-1083. e-mail: rafael.rosa@unifebe.edu.br
4Centro Universitário da Fundação Educacional de Brusque - UNIFEBE. Balneário Camboriú - SC, Brazil.
ORCID: https://orcid.org/0009-0009-5219-0129. e-mail: daniela.camargo@unifebe.edu.br
5Universidade Federal de Santa Catarina - UFSC. Brusque-SC, Brazil. ORCID: https://orcid.org/0000-0002-4171-9965. e-mail: fabila.rosa@unifebe.edu.br
Corresponding Author
Francis Marcos Bedin
Rua Pomerode, Número 101. Brusque-SC, Brazil. CEP: 88352-165. E-mail: francis.bedin@unifebe.edu.br Contato: +55 (49) 984038464.
Submission: 04-04-2025
Approval: 16-12-2025
ABSTRACT
Introduction: Systemic Arterial Hypertension (SAH) is recognized as a serious chronic medical condition, characterized by recurrent elevation of systolic blood pressure equal to or greater than 140 mmHg, or diastolic blood pressure equal to or greater than 90 mmHg, or by the use of antihypertensive medication. Objective: To understand the mechanisms through which systemic arterial hypertension may act as a determining factor in the development of intracerebral hemorrhages. Method: This is a theoretical–reflective study based on current scientific literature. Results: Systemic Arterial Hypertension, characterized by chronic elevation of blood pressure, promotes structural changes in cerebral blood vessels, such as hypertrophy of the medial layer and degeneration of the endothelial layer, making them more susceptible to spontaneous rupture. In addition, impairment of cerebral autoregulation in hypertensive patients favors hemorrhagic events, particularly in small arteries and deep arterioles. Intracerebral hemorrhage is one of the most severe complications, being associated with high morbidity and mortality, permanent neurological deficits, and a significant negative impact on patients’ quality of life. The management of hypertension, including continuous monitoring and effective therapeutic strategies, substantially reduces the risk of intracerebral hemorrhages and their consequences. Conclusion: Strict blood pressure control is essential as a primary and secondary prevention strategy for intracerebral hemorrhages. Furthermore, public health policies aimed at awareness and early treatment of systemic arterial hypertension are of paramount importance in minimizing its burden on the healthcare system.
Keywords: Hypertension; Cerebral Hemorrhage; Pathophysiology.
RESUMEN
Introducción: La Hipertensión Arterial Sistémica (HAS) es reconocida como una condición médica crónica grave, caracterizada por la elevación recurrente de la presión arterial sistólica igual o superior a 140 mmHg, o de la presión arterial diastólica igual o superior a 90 mmHg, o bien por el uso de medicación antihipertensiva. Objetivo: Comprender los mecanismos mediante los cuales la hipertensión arterial sistémica puede actuar como un factor determinante en el desarrollo de hemorragias encefálicas. Método: Se trata de un estudio teórico-reflexivo basado en la literatura científica actual. Resultados: Se identificó que la Hipertensión Arterial Sistémica, caracterizada por la elevación crónica de la presión arterial, promueve alteraciones estructurales en los vasos sanguíneos cerebrales, como la hipertrofia de la capa media y la degeneración de la capa endotelial, haciéndolos más susceptibles a rupturas espontáneas. Además, el deterioro de la autorregulación cerebral en pacientes hipertensos favorece episodios hemorrágicos, especialmente en pequeñas arterias y arteriolas profundas. La hemorragia intracerebral es una de las complicaciones más graves, asociándose a alta morbimortalidad, déficits neurológicos permanentes y un impacto significativo en la calidad de vida de los pacientes. El manejo de la hipertensión, incluyendo el monitoreo continuo y estrategias terapéuticas eficaces, reduce sustancialmente el riesgo de hemorragias encefálicas y sus consecuencias. Conclusión: Es imprescindible el control riguroso de la presión arterial como estrategia esencial en la prevención primaria y secundaria de las hemorragias encefálicas, así como la importancia de políticas públicas orientadas a la concienciación y al tratamiento precoz de la Hipertensión Arterial Sistémica para minimizar su carga sobre el sistema de salud.
Palabras clave: Hipertensión; Hemorragia Cerebral; Fisiopatología.
RESUMO
Introdução: A Hipertensão Arterial Sistêmica (HAS) é reconhecida como uma condição médica crônica grave, caracterizada pelo aumento recorrente da pressão sistólica igual ou superior a 140 mmHg, ou a pressão diastólica igual ou superior a 90 mmHg, ou ainda, quando há uso de medicação para hipertensão. Objetivo: compreender os mecanismos pelos quais a hipertensão arterial sistêmica pode atuar como um fator determinante para o desenvolvimento de hemorragias encefálicas. Método: trata-se de um estudo teórico-reflexivo baseado na literatura científica atual. Resultados: se identificou que a Hipertensão Arterial Sistêmica é caracterizada pela elevação crônica da pressão arterial, promove alterações estruturais nos vasos sanguíneos cerebrais, como hipertrofia da camada média, degeneração da camada endotelial, tornando-os mais suscetíveis a rupturas espontâneas. Além disso, a deterioração da autorregulação cerebral em pacientes hipertensos favorece episódios hemorrágicos, especialmente em pequenas artérias e arteríolas profundas. A hemorragia intracerebral é uma das complicações mais graves, estando associada a alta morbimortalidade, déficits neurológicos permanentes e significativo impacto na qualidade de vida dos pacientes. O manejo da hipertensão, incluindo monitoramento contínuo e estratégias terapêuticas eficazes, reduz substancialmente o risco de hemorragias encefálicas e suas consequências. Conclusão: é imprescindível o controle rigoroso da pressão arterial como estratégia essencial na prevenção primária e secundária das hemorragias encefálicas, bem como a importância de políticas públicas voltadas à conscientização e ao tratamento precoce da Hipertensão Arterial Sistêmica para minimizar sua carga sobre o sistema de saúde.
Palavras-chaves: Hipertensão; Hemorragia Cerebral; Fisiopatologia.
INTRODUCTION
Systemic Arterial Hypertension (SAH) is recognized as a serious chronic medical condition, characterized by a recurrent increase in systolic blood pressure equal to or greater than 140 mmHg, or diastolic blood pressure equal to or greater than 90 mmHg, or when using medication for hypertension. These determinants not only increase the risk of mortality from cardiovascular and renal diseases, but have also demonstrated a growing concern among peers in the field regarding the increased risk of developing dysfunctions associated with neurological perfusion(1).
Currently, it is estimated that 33% of individuals between 30 and 79 years of age worldwide are affected by this condition, with the number of hypertensive adults doubling from 650 million in 1990 to 1.3 billion in 2019, highlighting the urgent need for effective actions to address this public health challenge(2).
Chronic elevation of blood pressure above optimal parameters imposes an excessive burden on the arterial walls, compelling the myocardium to an excessively pronounced effort, culminating in damage to vital organs such as the brain, heart, and kidneys. The impact of hypertension on individuals' health is considerable; according to statistical surveys, in a global context, ischemic heart disease remains the leading cause of cardiovascular mortality, followed by intracerebral hemorrhage and ischemic stroke. In 2022, global deaths due to cardiovascular diseases increased from 12.4 million in 1990 to 19.8 million, reflecting global population growth and aging, as well as avoidable metabolic, environmental, and behavioral risks that contribute to this burden. These conditions are directly related to chronic hypertension (3).
Therefore, hypertension is associated with several complications, with cerebral hemorrhage being one of the most significant. Chronic elevated blood pressure exerts excessive forces on the walls of cerebral blood vessels, predisposing them to ruptures and hemorrhages. Understanding the mechanisms underlying this relationship is crucial for developing effective prevention and intervention strategies.
Therefore, this study aims to understand the mechanisms by which systemic arterial hypertension can act as a determining factor in the development of cerebral hemorrhages.
METHODS
This is a theoretical-reflective study, based on current scientific literature relevant to the topic. This work was generated from the provocations that occurred in the Academic League of Physiopathology, inherent to the Undergraduate Course in Medicine at the University Center of Brusque (UNIFEBE). Students of the Bachelor of Medicine course were tasked, as part of the evaluation process for the subject, with carrying out a critical and reflective analysis of the proposed theme.
RESULTS
PATHOPHYSIOLOGY OF SYSTEMIC ARTERIAL HYPERTENSION
Hypertension is a complex and multifactorial condition, marked by several structural and functional adaptations in the cardiovascular system, which contribute to persistently elevated blood pressure. A central aspect of this condition is vascular remodeling of the arterial walls, where chronic exposure to high blood pressure levels leads to hypertrophy of the smooth muscle of the arterioles, vessels responsible for regulating peripheral vascular resistance (PVR). This process, in turn, increases PVR, which is one of the main determinants of high blood pressure. In addition to the arterioles, the left ventricle of the heart also undergoes hypertrophy in response to the workload imposed by hypertension. This ventricular hypertrophy allows the heart to maintain adequate cardiac output under high pressure, but also increases myocardial oxygen demand (MVO2). In hypertensive patients, especially those with coronary artery disease, this increased demand can result in myocardial ischemia, compromising the contractile function of the heart and contributing to heart failure (4).
Blood pressure is the result of the combination of cardiac output (CO) and systemic vascular resistance (SVR); consequently, in the early stages of hypertension, both increased CO and SVR can be responsible for elevated blood pressure. In some individuals, especially young people, hypertension can manifest as hyperdynamic hypertension, characterized by increased cardiac output with relatively low SVR. Over time, arteriolar hypertrophy and increased SVR become the main factors maintaining hypertension. As arteriolar muscle hypertrophy progresses, the left ventricle faces increasing overload, leading to ventricular stiffness and decreased diastolic compliance. This impairs ventricular filling during diastole, reducing the heart's ability to increase output in response to physiological demands such as exercise or stress (5).
The sympathetic nervous system (SNS) plays a crucial role in blood pressure control, often presenting as hyperactive in patients with essential hypertension. Activation of the sympathetic nervous system (SNS) increases both cardiac output (CO) and systemic vascular resistance (SVR), contributing to elevated blood pressure. Because of this, hypertensive patients tend to exhibit increased baroreceptor sensitivity and elevated levels of catecholamines, such as norepinephrine, prolonging the hypertensive effects. Another relevant hormonal mechanism is the renin-angiotensin-aldosterone system (RAAS). Renin, released by the kidneys in response to decreased renal perfusion or sympathetic stimulation, converts angiotensinogen into angiotensin I, which is transformed into angiotensin II, a potent vasoconstrictor that increases SVR and stimulates the release of aldosterone by the adrenal glands. Aldosterone promotes sodium and water retention by the kidneys, increasing blood volume and, consequently, blood pressure (4).
Sodium sensitivity also plays an important role in the pathogenesis of hypertension. Individuals sensitive to sodium experience more pronounced increases in blood pressure in response to sodium intake, a condition more common in elderly populations, hypertensive patients with low renin, diabetics, and patients with renal insufficiency. Defects in renal sodium excretion contribute to fluid retention and elevated blood pressure. Concomitantly, obesity, especially central obesity, is another significant risk factor for hypertension. It is associated with metabolic syndrome, which includes insulin resistance, dyslipidemia, and sodium-sensitive hypertension. The relationship between obesity and hypertension is mediated by hemodynamic and hormonal changes, including activation of the SNS and the renin-angiotensin system (4).
In summary, hypertension is a complex condition resulting from a series of structural and functional adaptations in the cardiovascular system, such as hypertrophy of arterioles and the left ventricle, hemodynamic changes, sympathetic hyperactivity, and the influence of the renin-angiotensin-aldosterone system. Furthermore, factors such as sodium sensitivity and obesity also play crucial roles in the development of this condition(5).
Figure 1 – Flowchart of the Pathophysiology of Systemic Arterial Hypertension.
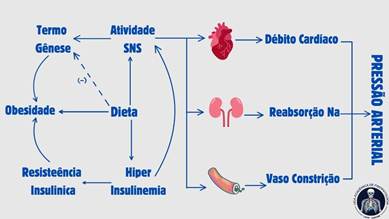 |
Source: Prepared by the authors, 2024.
HEMORRHAGIC EVENT CAUSED BY SYSTEMIC ARTERIAL HYPERTENSION.
Hemorrhagic events caused by systemic arterial hypertension (SAH) are a serious complication that occurs when excessive pressure in blood vessels leads to the rupture of arterial walls, resulting in bleeding in organs such as the brain, retina, or viscera. In the case of intracerebral hemorrhage, which accounts for 10 to 15% of strokes, mortality is high due to the destruction of brain tissue and increased intracranial pressure. Initial management includes rigorous blood pressure control, bleeding interruption, reversal of coagulopathies, and, in more severe cases, clot removal by surgical techniques. Adequate control of SAH is fundamental to preventing such hemorrhagic events, reducing the risk of fatal complications (6).
Spontaneous acute intracerebral hemorrhage (ICH) is a critical condition that represents a significant cause of overall morbidity and mortality. In the context of ICH, the primary hemorrhagic event occurs with the initial rupture of blood vessels, leading to the development of a hematoma. This primary bleeding can be exacerbated by high blood pressure, which increases the risk of hematoma expansion and, consequently, secondary hemorrhage. Hematoma expansion, associated with cerebral edema, frequently occurs within the first 24 hours and may require surgical intervention, such as decompressive craniectomy. Studies suggest that early and intensive reduction of blood pressure in patients with extremely high levels can improve functional recovery. Therefore, rapid diagnosis and appropriate treatment are crucial to minimize the impact of primary and secondary hemorrhage, providing better neurological outcomes and increasing the chances of recovery (7).
The expansion of the primary hematoma can also exert additional pressure on adjacent blood vessels, leading to new ruptures and an increase in bleeding volume. This secondary process is often aggravated by hypertension, which can intensify pressure on brain structures and increase the risk of complications such as cerebral edema and neurological deterioration (7).
Within the pathophysiological context, hypertension represents a significant predisposing factor for primary intraventricular hemorrhage (PIVH), a rare subtype of intraventricular hemorrhage without a hemorrhagic parenchymal component. PIVH can be caused by various conditions, such as trauma, vascular anomalies, and coagulation disorders, but hypertension stands out as the most common cause, followed by hemorrhages due to vascular anomalies. Hypertension can be both the direct cause of PIVH and act as a predisposing factor for bleeding in cases of associated vascular anomalies. Studies indicate that hypertensive PIVH should be diagnosed when there is elevated blood pressure on admission, negative cerebral angiography for vascular anomalies, and exclusion of other causes of intracranial hemorrhage. The prognosis is worse in patients with low Glasgow Coma Scale scores, advanced age, hydrocephalus, or more extensive intraventricular bleeding. In these cases, hemodynamic control is essential to prevent PIVH and avoid its associated complications(8).
Intracerebral hemorrhagic events, among other serious cerebrovascular accidents, are directly impacted by the deterioration of cerebral autoregulation, especially in patients with chronic hypertension. Cerebral autoregulatory impairment, which can persist after an acute ischemic stroke, increases the risk of hemorrhagic expansion and complications such as malignant cerebral edema, particularly in conditions affecting small vessels. These findings highlight the importance of closely monitoring cerebral autoregulatory function to adjust therapeutic strategies and improve neurological outcomes. Therefore, effective blood pressure management and continuous surveillance are essential to mitigate the risks of hemorrhagic events and promote more favorable neurological recovery. Implementing these measures can ultimately make a significant difference in the quality of life and clinical outcomes of hypertensive patients (9).
CLINICAL OUTCOME OF HYPERTENSION AND HEMORRHAGE
As previously mentioned, hypertension is a medical condition characterized by persistently elevated blood pressure, and is a significant risk factor for several cardiovascular complications, including hemorrhage. The relationship between hypertension and hemorrhage is complex and involves several pathophysiological mechanisms that culminate in varied clinical outcomes, depending on the severity and appropriate clinical management (10).
Furthermore, chronic hypertension can lead to the development of cerebral microangiopathy, a condition that weakens the smaller blood vessels in the brain, increasing the risk of micro-hemorrhages and cerebral lacunae. These vascular changes are frequently associated with cognitive impairment and dementia, highlighting the importance of blood pressure control in preventing neurological complications (10).
Subarachnoid hemorrhage (SAH) frequently results in severe impairment of cerebral metabolism and oxygenation, due to reduced cerebral blood flow (CBF) and dysfunction in cerebral autoregulation. Cerebral hypoxia resulting from vasospasm, which occurs in up to 70% of cases, is one of the main factors contributing to ischemia and neuronal damage. The imbalance between oxygen supply and demand in the brain exacerbates cell injury, especially in areas vulnerable to low perfusion (11,12).
Rebleeding occurs mainly in the first 24 hours after the hemorrhagic event and is associated with a high mortality and morbidity rate. Without proper management, such as early clipping or embolization of aneurysms, the risk of rebleeding can be fatal, with significant worsening of neurological deficits. The presence of hemorrhage is closely related to an exponential increase in intracranial pressure, exacerbating cerebral dysfunction (11,13).
Cerebral vasospasm is a critical complication that can occur between 4 and 14 days after SAH, and is related to prolonged constriction of cerebral blood vessels, reducing CBF. Delayed cerebral ischemia, caused by vasospasm, is a major cause of morbidity in SAH survivors. Treatment includes the use of vasodilating agents and volume control therapies to preserve cerebral perfusion and prevent secondary ischemic injuries (14,15).
Hydrocephalus occurs due to the accumulation of blood in the ventricular spaces, blocking the normal flow of cerebrospinal fluid (CSF). This condition leads to ventricular dilation and increased intracranial pressure, which can result in significant neurological deterioration if left untreated. Ventricular shunting is often necessary to relieve pressure and restore CSF balance (12,14).
Seizures are a frequent complication after intracranial hemorrhages, especially in patients with ruptured aneurysms. Metabolic changes, inflammation, and the irritating effects of extravasated blood on brain tissue are predisposing factors for epileptic seizures. The use of anticonvulsants, such as phenytoin or levetiracetam, may be necessary for seizure prophylaxis and improved prognosis (16,17).
The clinical outcomes of hypertension and hemorrhage depend not only on the effectiveness of blood pressure control, but also on the timing of the intervention and multimodal treatment, which may include pharmacological measures, intensive support, and rehabilitation. Interdisciplinary and personalized management is essential to optimize outcomes and improve the quality of life of patients affected by these conditions (18).
FINAL CONSIDERATIONS
Systemic arterial hypertension (SAH) causes structural and functional changes in the arteries, such as thickening and stiffening of the vascular walls, a phenomenon known as arteriosclerosis. This loss of elasticity compromises the ability of vessels to adapt to pressure variations, overloading the cardiovascular system and increasing the risk of vascular rupture, especially in organs such as the brain and eyes.
Hemorrhagic events resulting from SAH are triggered by the inability of damaged blood vessels to withstand increased pressure. Chronic hypertension affects cerebral autoregulation, contributing to intracerebral and primary intraventricular hemorrhages (PIVH). In these conditions, inadequate blood pressure control worsens the prognosis, favoring the expansion of bleeding and increasing the risk of secondary complications, such as cerebral ischemia.
The clinical outcome in patients with hemorrhages associated with hypertension is generally severe, especially in cases of intracerebral hemorrhage, where hematoma enlargement is linked to higher mortality and worsening functional status. Early intervention to reduce blood pressure has been shown to limit hematoma expansion and reduce mortality. However, the impact on long-term functional recovery still requires further study. Effective blood pressure control is crucial, as inadequate management can result in permanent neurological sequelae, such as cognitive and motor deficits. Therefore, rigorous multidisciplinary management of hypertension, including continuous monitoring and appropriate pharmacological treatment, is essential to optimize outcomes, prevent rebleeding, and ensure the best possible quality of life for patients.
REFERENCES
1. Lima TE, Bonadio AC, Nunes PLP, Boleta-Ceranto D de CF. Hypertension: a systematic review. Brazilian Journal of Health Review [Internet]. 2021 [cited 2024 Mar 14]5;4(4):16417–27. Available from: https://doi.org/10.34119/bjhrv4n4-158
2. World Health Organization. Global report on hypertension: the race against a silent killer [Internet]. Available from: https://www.who.int/publications/i/item/9789240081062
3. Walther O. New Study Reveals Latest Data on Global Burden of Cardiovascular Disease [Internet]. American College Cardiol. 2023. Available from: https://www.acc.org/About-ACC/Press-Releases/2023/12/11/18/48/New-Study-Reveals-Latest-Data-on-Global-Burden-of-Cardiovascular-Disease
4. Sanjuliani AF. Fisiopatologia da hipertensão arterial: conceitos teóricos úteis para a prática clínica. Rev SOCERJ [Internet]. 2002 [cited 2024 Mar 14]15(4):210-218. Available from: http://sociedades.cardiol.br/socerj/revista/2002_04/a2002_v15_n04_art02.pdf
5. Nocite JR. Fisiopatologia da hipertensão arterial e avaliação do paciente hipertenso. Rev. Bras. Anestesiol [Internet]. 1988 [cited 2024 Mar 14]38(4):257-62. Available from: http://www.rba.periodikos.com.br/article/5e498b5e0aec5119028b45e3/pdf/rba-38-4-257.pdf
6. Rocha E, Rouanet C, Reges D, Gagliardi V, Singhal AB, Silva GS. Intracerebral hemorrhage: update and future directions. Arquivos de Neuro-Psiquiatria [Internet]. 2020 [cited 2024 Mar 14]78(10):651-659. Available from: https://doi.org/10.1590/0004-282X20200088
7. Bombig MTN, Francisco YA, Bianco HT. Acidente vascular cerebral e hipertensão: relação, metas e recorrência. Rev Bras Hipertens [Internet]. 2021 [cited 2024 Mar 14]28(3):232-7. Available from: http://dx.doi.org/10.47870/1519-7522/20212803232-7
8. Robles LA, Volovici V. Hypertensive primary intraventricular hemorrhage: a systematic review. Neurosurgical review [Internet]. 2022 [cited 2024 Mar 14]45(3):2013-2026. Available from: https://doi.org/10.1007/s10143-022-01758-8
9. Al-Kawaz M, Cho SM, Gottesman RF, Suarez JI, Rivera-Lara L. Impact of cerebral autoregulation monitoring in cerebrovascular disease: a systematic review. Neurocritical care [Internet]. 2022 [cited 2024 Mar 14]36(3):1053-70. Available from: https://doi.org/10.1007/s12028-022-01484-5
10. Iadecola C, Yaffe K, Biller J, Bratzke LC, Faraci FM, Gorelick PB et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension [Internet]. 2016 [cited 2024 Mar 14]68(6):e67-e94. Available from: https://doi.org/10.1161/HYP.0000000000000053
11. Huttunen J, Kurki MI, von und zu Fraunberg M, Koivisto T, Ronkainen A, Rinne J et al. Epilepsy after aneurysmal subarachnoid hemorrhage: a population-based, long-term follow-up study. Neurology [Internet]. 2015 [cited 2024 Mar 14]84(22):2229-37. Available from: https://doi.org/10.1212/WNL.0000000000001643
12. Dennis M, Fitz CR, Netley CT, Sugar J, Harwood-Nash DC, Hendrick EB et al. The intelligence of hydrocephalic children. Archives Neurol [Internet]. 1981 [cited 2024 Mar 14]38(10):607-15. Available from: https://doi.org/10.1001/archneur.1981.00510100035004
13. Kim DH, Dunn IF. Three-Day Phenytoin Prophylaxis is Adequate after Subarachnoid Hemorrhage. Neurosurgery [Internet]. 2007 [cited 2024 Mar 14]61(6):p E1340. Available from: https://doi.org/10.1227/01.neu.0000306134.28732.62
14. Moussouttas M, Lai EW, Dombrowski K, Huynh TT, Khoury J, Carmona G et al. CSF catecholamine profile in subarachnoid hemorrhage patients with neurogenic cardiomyopathy. Neurocritical care [Internet]. 2011 [cited 2024 Mar 14]14(3):401-06. Available from: https://doi.org/10.1007/s12028-011-9527-6
15. Lee VH, Oh JK, Mulvagh SL, Wijdicks EF. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocritical care [Internet]. 2006 [cited 2024 Mar 14]5(3):243-49. Available from: https://doi.org/10.1385/NCC:5:3:243
16. Claassen J, Perotte A, Albers D, Kleinberg S, Schmidt JM, Tu B et al. Nonconvulsive seizures after subarachnoid hemorrhage: multimodal detection and outcomes. Annals neurol [Internet]. 2013 [cited 2024 Mar 14]74(1):53-64. Available from: https://doi.org/10.1002/ana.23859
17. Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocritical care [Internet]. 2010 [cited 2024 Mar 14]12(2):165-72. Available from: https://doi.org/10.1007/s12028-009-9304-y
18. Morgenstern LB, Hemphill III JC, Anderson C, Becker K, Broderick JP, Connolly Jr ES et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke [Internet]. 2010 [cited 2024 Mar 14]41(9):2108-29. Available from: https://doi.org/10.1161/STR.0b013e3181ec611b
Declaration of Conflict of Interest:
Nothing to declare.
Funding and Acknowledgments:
No funding.
Authorship Criteria (Author Contributions):
1. Substantially contributes to the conception and/or planning of the study; João Victor Bassan do Nascimento, Francis Marcos Bedin, Rafael Schmitt da Rosa, Daniela Lima de Camargo, Fábila Fernanda dos Passos da Rosa.
2. Obtaining, analyzing, and/or interpreting the data; João Victor Bassan do Nascimento, Francis Marcos Bedin, Rafael Schmitt da Rosa, Daniela Lima de Camargo, Fábila Fernanda dos Passos da Rosa.
3. Writing and/or critically revising and final approval of the published version. João Victor Bassan do Nascimento, Francis Marcos Bedin, Rafael Schmitt da Rosa, Daniela Lima de Camargo, Fábila Fernanda dos Passos da Rosa.
Scientific Editor: Ítalo Arão Pereira Ribeiro. Orcid: https://orcid.org/0000-0003-0778-1447
Rev Enferm Atual In Derme 2026;100(1): e026015