REVIEW
ARTICLE
PREDICTIVE
INDICATORS OF PRESSURE INJURIES IN HOSPITALIZED ADULTS AND ELDERLY PEOPLE:
INTEGRATIVE REVIEW
INDICADORES
PREDICTIVOS DE LESIONES POR PRESIÓN EN ADULTOS Y ANCIANOS HOSPITALIZADOS:
REVISIÓN INTEGRATIVA
INDICADORES
PREDITIVOS DA LESÃO POR PRESSÃO EM ADULTOS E IDOSOS HOSPITALIZADOS: REVISÃO
INTEGRATIVA
https://doi.org/10.31011/reaid-2025-v.99-n.1-art.2301
1Natália Chantal Magalhães da Silva
2João Pedro Teixeira Marcos
3Sônia Regina de Souza
4Alcione Matos de Abreu
5Rosane de Paula Codá
1Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, Brazil. ORCID: https://orcid.org/0000-0003-1883-4313.
2Secretaria Municipal de Saúde do Rio de
Janeiro, Rio de Janeiro, Brasil. ORCID: https://orcid.org/0009-0007-5238-2388.
3Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, Brazil. ORCID: https://orcid.org/0000-0001-7981-0038.
4Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, Brazil. ORCID: https://orcid.org/0000-0001-6078-7149.
5Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, Brazil. ORCID: https://orcid.org/0000-0002-9881-1543.
Autor
correspondente
Natália
Chantal Magalhães da Silva
Departamento
de Enfermagem Médico-Cirúrgica – DEMC/EEAP/UNIRIO. (Rua Xavier Sigaud, 290, Rio
de Janeiro - Brazil. CEP: 222290-180), Tel: +55(021) 996040364. E-mail: natalia.c.silva@unirio.br.
Submission: 26-06-2024
Approval: 19-02-2025
ABSTRACT
Objective: To present the
knowledge produced about the predictive indicators of pressure injuries in
hospitalized adults and elderly people. Method: Integrative review of the
literature, carried out based on PRISMA recommendations, with the guiding
question: “What knowledge is produced about the predictive indicators of
pressure injuries in hospitalized adults and elderly people?”. The searches
were carried out in Latin American and Caribbean Literature in Health Sciences,
CAPES Journal Portal and National Library of Medicine. Results: 43 studies
comprised this review. In 42, the use of a single evaluation method was
observed, with a predominance of evaluation instruments: Braden Scale (n = 37,
86%); followed by the Waterlow Scale (n = 7, 16.2%); and, Norton Scale (n = 6,
13.9%). Only a single study (2.3%) used combined assessment methods: different
instruments and presence of comorbidities. In two studies, the assessment took
place through the analysis of a specific clinical aspect (nutritional status).
Conclusions: The main predictive indicators for assessing the risk of pressure
injuries in hospitalized adults and elderly people come from assessment
instruments. However, it is suggested that research be developed aimed at
analyzing the reliability and validation of such instruments in specific
populations.
Keywords:
Pressure Injury; Elderly Health; Adult Health; Hospitalization.
RESUMEN
Objetivo: Presentar el
conocimiento producido sobre los indicadores predictivos de lesiones por
presión en adultos y ancianos hospitalizados. Método: Revisión integradora de
la literatura, realizada con base en las recomendaciones PRISMA, con la
pregunta orientadora: “¿Qué conocimiento se produce sobre los indicadores
predictivos de lesiones por presión en adultos y ancianos hospitalizados?”. Las
búsquedas se realizaron en Literatura Latinoamericana y del Caribe en Ciencias
de la Salud, Portal de Revistas CAPES y Biblioteca Nacional de Medicina.
Resultados: 43 estudios comprendieron esta revisión. En 42 se observó el uso de
un único método de evaluación, con predominio de los instrumentos de
evaluación: Escala de Braden (n = 37, 86%); seguida de la Escala de Waterlow (n
= 7, 16,2%); y Escala de Norton (n = 6, 13,9%). Sólo un estudio (2,3%) utilizó
métodos de evaluación combinados: diferentes instrumentos y presencia de
comorbilidades. En dos estudios, la evaluación se realizó mediante el análisis
de un aspecto clínico específico (estado nutricional). Conclusións: Los
principales indicadores predictivos para evaluar el riesgo de lesiones por
presión en adultos y ancianos hospitalizados provienen de instrumentos de
evaluación. Sin embargo, se sugiere desarrollar investigaciones dirigidas a
analizar la confiabilidad y validación de dichos instrumentos en poblaciones
específicas.
Palabras-clave:
Lesión por presión; Salud de las personas mayores; Salud del Adulto;
Hospitalización.
RESUMO
Objetivo: Apresentar o conhecimento produzido sobre os
indicadores preditivos da lesão por pressão em adultos e idosos hospitalizados.
Método: Revisão integrativa da literatura, realizada a partir das recomendações
PRISMA, tendo como questão norteadora: “Qual o conhecimento produzido sobre os
indicadores preditivos da lesão por pressão em adultos e idosos
hospitalizados?”. As buscas foram realizadas na Literatura Latino-Americana e
do Caribe em Ciências da Saúde, Portal de Periódicos CAPES e National Library
of Medicine. Resultados: 43 estudos compuseram esta revisão. Em 42, foi
observado o emprego de um único método avaliativo, com predomínio dos
instrumentos de avaliação: Escala de Braden (n = 37, 86%); seguida da Escala de
Waterlow (n = 7, 16,2%); e, Escala de Norton (n = 6, 13,9%). Apenas um único
estudo (2,3%) utilizou métodos avaliativos combinados: instrumentos distintos e
presença de comorbidades. Em dois estudos, a avaliação se deu por meio da
análise de um aspecto clínico específico (estado nutricional). Conclusões: Os
principais indicadores preditivos para avaliação do risco de lesão por pressão
em adultos e idosos hospitalizados são provenientes de instrumentos de
avaliação. Sugere-se, contudo, o desenvolvimento de pesquisas voltadas para a
análise da confiabilidade e validação de tais instrumentos em populações
específicas.
Palavras-chave: Lesão
por Pressão; Saúde do Idoso; Saúde do Adulto; Hospitalização.
INTRODUCTION
The motivation for
developing this study arose during the Undergraduate Nursing Course, more
specifically in practical teaching and extension activities focused on adult
and elderly health and injury care. Empirically, it was observed that pressure
injuries were present in hospitalized patients in the most diverse sectors,
such as medical and surgical clinics, orthopedics, urology, gynecology, among
others.
Recognized as an adverse
health event and, sometimes, as a negative indicator of the quality of care,
pressure injuries should be the focus of knowledge and updating by nursing
professionals, especially with regard to predictive indicators of their
appearance (¹).
This type of injury is
defined by the National Pressure Ulcer Advisory Panel (NPUAP) and the European
Pressure Ulcer Advisory Panel (EPUAP) as “localized injury to the skin and/or
underlying tissue over a bony prominence as a result of pressure or pressure in
combination with shear and/or friction” (2,3). Regarding the degree
of impairment, it can be classified as: grade 1, with the presence of intact
skin with non-blanchable hyperemia; grade 2, with partial skin loss, exposure
of the dermis or blister with serous content; grade 3, with total skin loss and
exposure of the subcutaneous tissue, which may present granulation, slough and
necrosis; and, grade 4, with total skin loss and exposure of other structures (2-4).
In addition to the costs
related to the health system, patients, families and the community are
significantly affected by physical, social and economic consequences (5).
Specifically in patients, the impact occurs in a relevant way in terms of pain
and negative self-image, worsening of quality of life, psychological trauma and
increased length of hospital stay (6).
Therefore, the
recognition of predictive factors of pressure injury allows the evaluation and
detection of characteristics that suggest some type of change in the skin,
which can be considered a warning sign for the appearance and installation of
the injury (7).
In addition to nursing
classification systems, such as NANDA-I (8) and ICNP (9),
which standardize several phenomena, especially those related to the risk of
pressure injury, some assessment instruments – such as the Braden Scale, Norton
Scale, Waterlow Scale, and Gosnell Scale – are widely used in clinical practice
aimed at hospitalized adults and elderly individuals (5).
In this context, by
gathering the knowledge produced on the predictive indicators of pressure
injury, it is possible to increase nursing action in the prevention of pressure
injuries, precisely because they are one of the most common preventable
complications during hospitalization (6).
Therefore, there is a
need for a more detailed and current look at the subject, recognizing the
relevance of prevention in nursing care. Therefore, the objective of this
research is to present the knowledge produced on the predictive indicators of
pressure injury in hospitalized adults and elderly individuals.
METHODS
This is an integrative
literature review, developed between April and June 2024, following the PRISMA
recommendations (10).
The purpose of this type of
review is to synthesize the knowledge already produced on the subject studied (11).
Thus, through the PCC strategy
– P: Population (adults and elderly); C: Concept (predictive indicators of
pressure injury); C: Context (hospitalization) – the guiding question was
elaborated: “What knowledge is produced on the predictive indicators of
pressure injury in hospitalized adults and elderly?”.
Searches were carried out in the
following databases: Latin American and Caribbean Literature in Health Sciences
(LILACS), CAPES Periodicals Portal (CAPES) and National Library of Medicine
(NLM) (PubMed), based on the search strategies presented in Table 1.
Table 1 – Search
strategies used in the databases.
|
DATABASE
|
SEARCH STRATEGIES
|
|
LILACS
|
Pressure
Injury AND Elderly Health [Subject Descriptor] OR Adult Health AND
Hospitalization [Subject Descriptor]
|
|
CAPES
|
Pressure
Injury and Adult [Subject Descriptor] and Hospitalization [Subject
Descriptor]
|
|
PubMed
|
((Pressure Ulcer [MeSH Terms]) AND
(Adult Health [MeSH Terms]) AND (Middle Aged [MeSH Terms]) AND
(Hospitalization [MeSH Terms]))
|
Source: Prepared by the authors.
The following inclusion
criteria were considered: articles available in full text, with free access,
published in the last 10 years, in Portuguese, Spanish and English. Duplicates
were excluded, considering the first indexed database.
For the best methodological
organization, a protocol was developed to guide the development of the
integrative review. Thus, after identifying the findings in the databases and
applying the limits, a selective analysis was carried out, with reading of the
title and abstract of the articles. Next, a critical analysis was performed,
with analysis of the response to the proposed guiding question (11).
The articles included in
the review had their identification data (database, reference, title, authors,
year of publication and country of publication), general characteristics
(objectives, methods, population, results and conclusions) and specific
characteristics (indicators used in the assessment of the skin seeking to
prevent pressure injuries; definition of these indicators; measurement of these
indicators; and characteristics and values indicative of normality and skin
alteration, seeking to prevent pressure injuries in hospitalized adults and
elderly people) tabulated in a Microsoft Excel spreadsheet, version 2023.
The analysis of the level
of evidence of the studies followed the method proposed by Melnyk and
Fineout-Overholt (12), which classifies them into: Level I, when it
is a systematic review or meta-analysis of randomized controlled clinical
trials; Level II, well-designed randomized controlled clinical trial; Level
III, well-designed clinical trial without randomization; Level IV,
well-designed cohort and case-control studies; Level V, systematic review of
descriptive and qualitative studies; Level VI, evidence derived from a single
descriptive or qualitative study; Level VII, opinion of authorities and/or
expert committees.
RESULTS
Initially, 989 articles were
identified; however, through the application of the eligibility criteria, 244
were considered. After selective and critical analysis, 43 articles comprised
this review – 36 (83.7%), indexed in PubMed; three (7%), in LILACS; and four
(9.3%) in CAPES (FIGURE 1).
Figure 1 - Flowchart of
article selection prepared based on PRISMA¹⁰ recommendations.
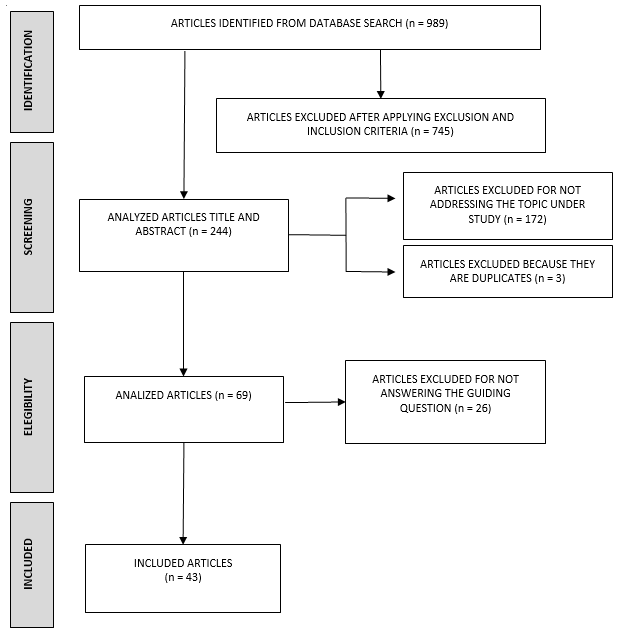
Source:
Prepared by the authors.
Of the 43 studies included in
this review, most were published in the last five years (74.4%); in Asia
(37.2%) and North America (37.2%) – with only five publications (11.6%)
identified in Brazil.
With regard to predictive
indicators of pressure injuries in hospitalized adults and elderly individuals,
42 studies used a single assessment method. In these, the following assessment
instruments predominated: Braden Scale (n = 37, 86%); followed by the Waterlow
Scale (n = 7, 16.2%); and the Norton Scale (n = 6, 13.9%). In two studies
(4.6%), the assessment was performed through the analysis of a specific
clinical aspect – in this case, nutritional status. Only one study (2.3%) used
combined assessment methods, namely: BWAT (Bates-Jensen Wound Assessment Tool),
PUSH (Pressure Ulcer Scale For Healing), PrePURSE (Pressure Ulcer Risk Score
Evaluation), Cubbin-Jackson Scale, Gosnell Scale, PURPOSE-T (Primary or
Secondary Pressure Ulcer Risk Assessment Tool) and presence of comorbidities
(TABLE 1).
Table 1 – Predictive
indicators of pressure injury in hospitalized adults and elderly people.
|
REFERENCES
|
PREDICTIVE
INDICATORS OF PRESSURE INJURY
|
|
Aghazadeh
et al., 2020 (5) ; Aloweni et al., 2018 (13) ; Bai et
al., 2020(14); Bereded & Salih & Abebe, 2018(15);
Brophy et al., 2021(16); Chaboyer et al. 2017(17);
Cortés et al, 2018(18); Cox et al., 2022(19); Debon et
al., 2018(20); Díaz-Icaro & Gómez-Heras, 2020(21);
Edsberg et al., 2022(22); Farias & Queiroz, 2022(23);
Garcia et al., 2021(24); Gupta et al. 2020(6); Ham et
al., 2016(25); Ho et al., 2017(26); Hyun et al., 2013(27);
Jiang et al. 2014(28); Jiang et al., 2020(29); Labeau
et al., 2020(30); Lee et al., 2019(31); Linnen et al.,
2018(32); Liu et al., 2019(33); Lopes et al., 2020(34);
Moreira & Simões & Ribeiro, 2020(2); Mutair et al., 2019(35);
Oe et al., 2020(36); Padula et al., 2016(37); Pickham
et al., 2018(38); Rashvand et al., 2019(4); Santamaria
et al., 2013(39); Serpa et al., 2020(40); Sousa &
Kapp & Santamaria, 2020(41); Shaw et al., 2014(42);
Wang et al., 2014(43); Yoshimura et al., 2016(44); Yoshimura
et al., 2020(45).
|
Braden Scale
|
|
Brophy
et al., 2021(16); Chaboyer et al., 2017(17); Díaz-Caro
& Gómez-Heras, 2020(21); Jiang et al., 2020(29); Lovegrove
& Fulbrook & Miles, 2018(46); Smith et al., 2017(47);
Sternal & Wilczyński & Szewieczek, 2016(48); Wang et al.,
2014(43).
|
Waterlow Scale
|
|
Cox
et al., 2022(19); Díaz-Caro & Gómez-Heras, 2020(21);
Jiang et al., 2014(28); Jiang et al., 2020(29); Schoeps
& Tallberg & Gunningberg, 2016(49); Wang et al., 2014(43);
|
Norton Scale
|
|
Díaz-Caro
& Gómez-Heras, 2020(21).
|
Gosnell Scale
|
|
Cox
et al., 2022(19).
|
Cubbin-Jackson Scale
|
|
Macedo
et al., 2021(1).
|
BWAT
(Bates-Jensen Wound Assessment Tool)
|
|
Macedo
et al., 2021(1).
|
PUSH
(Pressure Ulcer Scale For Healing)
|
|
Aloweni
et al., 2018(13).
|
PrePURSE
(Pressure Ulcer Risk Score Evaluation)
|
|
Cheng
et al., 2020(50).
|
PURPOSE-T
(Primary or Secondary Pressure Ulcer Risk Assessment Tool)
|
|
Gupta
et al., 2020(6); Santamaria et al., 2013(39).
|
Nutritional status
|
|
Santamaria
et al., 2013(39).
|
Presence of comorbidities
|
Eleven
studies (25.5%) presented conceptual definitions of predictive indicators (1,13-22);
18 (41.8%) revealed methodological details regarding the application of
indicators (1,2,4-5,13-14,17,20-30); and 21 (48.8%) cited the
indicative standards of normality (1,2,5,13,15-16,19,21,23,24,26,30-39).
In this
sense, the Braden Scale, applied in 15 studies (34.9%), can be defined as a
valid and easy-to-apply instrument that allows qualifying and quantifying the
etiological factors for reduced tissue tolerance to prolonged compression (13-14,20,23,31-32,38,40).
Composed of six subscales (sensory perception, skin moisture, activity,
mobility, nutrition, and friction and shear), each of which can be assigned
from 1 to 3 or 4 points, scoring a total that varies from 6 to 23 points –
where the lowest score indicates greater risk and the highest score indicates
greater risk (20).
Similarly,
the Cubbin-Jackson Scale, identified in one study (2.3%), considers, in
addition to factors similar to the Braden Scale such as mobility, nutrition,
and sensory perception, also oxygenation in its risk scale (19).
As for
the Norton Scale, it was applied in three studies (7%), however, the definition
of the instrument was not presented. However, it is known that it consists of
five subscales (physical condition, mental condition, activity, mobility and
continence), which can receive from 1 to 4 points, where 1 indicates the worst
quality indicator and 4 the best quality indicator – totaling up to 20 points (21,28,43,49).
The
Waterlow Scale, present in one study (2.3%), is considered an instrument that
categorizes the level of risk of pressure injury through a management plan for
guidance and recording of the interventions (46). It consists of
seven items, namely: weight and height ratio (BMI), skin type, sex and age,
degree of malnutrition, continence, mobility and special risk factors, with
scores ranging from 1 to 64. As an example, patients with a score between 10
and 14 were at risk; between 15 and 19, high risk; and above 20, very high risk
(17,43,48).
Similarly,
the Bates-Jensen Wound Assessment Tool (BWAT) scale, used in one study (2.3%),
was defined as a long scale that thoroughly assesses the existing injury. It
has 13 items that assess size, depth, edges, detachment, type and quantity of
necrotic tissue, type and quantity of exudate, edema and hardening of
peripheral tissue, skin color around the pressure injury, granulation tissue
and epithelialization - the assessment is performed using a five-point scale,
where 1 indicates the best condition of the wound and 5, the worst condition.
The total score of the scale is obtained by adding all items and can range from
13 to 65 points, with higher scores indicating the worst condition of the
pressure injury (1).
The
PUSH Scale (Pressure Ulcer Scale for Healing, present in one article (2.3%), is
defined as a short and easy-to-apply scale. Basically, it consists of three
parameters for evaluating the healing process and intervention results: area,
amount of exudate and appearance of the pressure injury bed. The scores of
these parameters, when added together, generate a total score that can range
from 0 to 17, with higher scores indicating worse conditions of the injury and
lower scores indicating improvement in the healing process (1).
The
PURPOSE-T Scale (Primary or Secondary Pressure Ulcer Risk Assessment Tool),
used in one study (2.3%), is considered a comprehensive structure for assessing
the risk of pressure injury, distinguishing primary and secondary factors (50).
The
Pressure Ulcer Risk Score Evaluation (prePURSE), used in one study (2.3%),
consists of five items that predict the risk of pressure injury: age, weight at
admission, abnormal skin appearance, friction/shearing problem and surgery next
week (13).
Regarding
the level of evidence, 26 (60.5%) were classified as Level IV; nine (21%) as
Level VI; three (7%) as Level I; two (4.6%) as Level II; two (4.6%) as Level
VII; and one (2.3%) as Level III, according to Melnyk; Fineout-Overholt (12).
DISCUSSION
In the scientific
literature, there is some difficulty in establishing a consensus regarding
predictive indicators of pressure injuries in hospitalized adults and elderly
individuals. There is a wide range of scales, instruments and clinical
indicators that consider basic and specific dimensions in this assessment.
Therefore, it is necessary to choose at least one tool that is appropriate for
the intended assessment, with the context of application and the sensitivity of
that predictive factor as a guiding element, given that reliable instruments
interfere with the reliability of the assessments (5-14,20,23,27-28,31-32,38,40,46,50).
Adequately inspecting the
skin plays a vital role in preventing pressure injuries, allowing the detection
of early signs (6). Poor nutritional status is a contributing factor
to the development of the injury; aging, humidity, shear and friction forces,
immobility and hospitalizations for long periods of time are extrinsic and
intrinsic factors for its formation, which is consistent with the results of
this article (6-7).
The rate of pressure
injuries is a measure of patient safety and an indicator of the quality of
nursing care (51). In order to reflect macroscopically on the
impacts of pressure injuries in a global aspect, we will analyze their effects
and relevance. The emergence of this type of injury significantly increases
health costs, mainly due to the use of dressings, support surfaces, increased
availability of nursing care time and medications (6). In Europe,
the prevalence of pressure injuries ranges from 4.6% to 27.2%; in Australia, 3%
for inpatient wards and 11.5% for intensive care units; in China, there is a
prevalence of 3.38% in hospitals (11). More than 2.5 million
patients in the United States develop pressure injuries, cumulatively costing
approximately US$9 to 11 billion for treatment and resulting in 60,000 deaths
from their complications each year (52).
Comparing hospital
expenses, another study revealed that they are significantly higher associated
with the presence of pressure injuries in the United States, with an average of
$128,997 in costs for patients who have them and $78,454 for patients without
the presence of pressure injuries (53). Considering countries with
less affluent health systems, their prevalence is higher, as in the case of
Brazil with 40% in hospital emergency units and Ethiopia with 14.9% (11).
In past studies in Brazil, there was a certain variation among hospitalized
patients who developed pressure injuries, both in profile and environment,
11.0% to 30.9% in intensive care units, 13.6% to 31.4% in surgical/clinical
units (40), however, there are still discrepancies between the data
found regarding the prevalence of these injuries.
When collecting relevant
data regarding the international and national impacts of pressure injuries in
hospitalized adults and elderly people, some limitations were identified for
the preparation of this integrative review. One notable point was the scarcity
of studies on the impact on actual health costs in the Brazilian health system (54).
Studies on predictive indicators of pressure injuries in this population are
minimally found, since the main approach is to treat wounds after they have
already developed (54,15). Studies also reveal the ease of
investigating the subject only in high- and middle-income countries; however,
there is a deficiency in production regarding low-income or underdeveloped
countries, even though they have higher prevalence of injuries in this
population, such as Brazil, Thailand and Ethiopia with significant rates of
12.7%, 47.6% and 16% respectively (15). In addition to the lack of
publications, the high volatility of financial data, prevalence, and incidence
were a challenge. The profile of PI development in intensive care is 11.0% to
30.9% and in surgical/clinical units 13.6% to 31.4%, as already mentioned in
Brazil, and 2 to 26% in mixed environments in Canada (15,17,19,21-23,25,27-29,30,33-35,40-43,47-49,51-54),
which is an impasse for an accurate determination of these data. Regarding
incidence, there are variations from 23.1% to 59.5% in Brazil according to one
author and from 0.4% to 38%, according to another. In addition to these
instabilities, there is also a noticeable incompatibility between authors (1,54).
The following limitations
were considered in this review: the time frame and the delimitation of
publications in Portuguese, English, and Spanish.
CONCLUSIONS
By analyzing the
scientific literature, this review gathered 43 findings that address the
predictive indicators of pressure injuries in hospitalized adults and elderly
individuals.
In 42 studies, the use of
a single assessment method was observed, with a predominance of assessment
instruments: Braden Scale (n = 37, 86%); followed by the Waterlow Scale (n = 7,
16.2%); and, Norton Scale (n = 6, 13.9%). Only one study (2.3%) used combined
assessment methods: different instruments and presence of comorbidities. In two
studies, the assessment was carried out through the analysis of a specific
clinical aspect (nutritional status).
In this review, the
impact of the use of predictive factors on health system costs, as well as
other repercussions related to the hospital context, was not identified.
Although there is consensus on the positive effects of early detection and
prevention of injuries on quality of life, length of hospital stay, bed
occupancy and cost reduction, the need for research aimed at analyzing the
cost-effectiveness of the factors discussed here is highlighted. Furthermore,
it is suggested that studies be carried out to assess the reliability and
validation of the instruments and other assessment methods mentioned above in
specific populations. This will help to mitigate misinterpretations and ensure
the reliability of the findings.
However, it is believed
that by presenting the knowledge produced about the predictive indicators of
pressure injuries, this research presents an extensive contribution not only to
clinical and scientific practice in the area of nursing, but to all those
involving the health of adults and the elderly, whether at the level of care or
management.
REFERENCES
- Macedo ABT, Graciotto A, Souza E, Junges M,
Gentilini MM, Souza SBC de. Pressure ulcers: correlation between the
bates-jensen wound assessment tool and the pressure ulcer scale for
healing. Texto contexto - enferm [Internet]. 2021;30:e20200260. Disponível
em: https://doi.org/10.1590/1980-265X-TCE-2020-0260
- Moreira MGS,
Simões SM, Ribeiro CJN. Perfil clínico-laboratorial de pacientes
hospitalizados acometidos por lesão por pressão. Estima – Braz J
Enterostomal Therapy. 2020 Nov 5;18. Disponível em: https://www.revistaestima.com.br/estima/article/view/885/339
- Kim JY, Lee YJ. Medical device‐related pressure
ulcer (MDRPU) in acute care hospitals and its perceived importance and
prevention performance by clinical nurses. Int Wound J. 2019;16:51-61.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7948724/
- Rashvand F, Shamekhi L, Rafiei H, Nosrataghaei M.
Incidence and risk factors for medical device-related pressure ulcers: The
first report in this regard in Iran. Int. Wound J. 2019;17:436-442.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7948845/
- Aghazadeh A, Lotfi M, Asgarpour H, Khajehgoodari
M, Nobakht A. Frequency and risk factors of pressure injuries in clinical
settings of affiliated to Tabriz University of Medical Sciences. Nurs
Open. 2020 Nov 15;8(2):808–14. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7877138/
- Gupta P, Shiju S, Chacko G, Thomas M, Abas A,
Savarimuthu I et al. A quality improvement programme to reduce
hospital-acquired pressure injuries. BMJ Open Qual. 2020;9:e000905.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7394182/
- Getie A, Baylie A, Bante A, Geda B, Mesfin F.
Pressure ulcer prevention practices and associated factors among nurses in
public hospitals of Harari regional state and Dire Dawa city administration,
Eastern Ethiopia. Serra R, editor. Plos One. 2020;15(12):e0243875.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7737888/
- Herdman H. NANDA International Nursing Diagnoses:
definitions& classification. 12th ed. Thieme Medical Publishers; 2021.
- Garcia TR (org.). Classificação Internacional
para a Prática de Enfermagem CIPE® versão 2020. Porto Alegre: Artmed;
2020.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I,
Hoffmann TC, Mulrow CD, et al. A declaração PRISMA 2020: diretriz
atualizada para relatar revisões sistemáticas. Epidemiol Serviços Saúde
[Internet]. 2022 Jun 1;31(2). Disponível em: http://scielo.iec.gov.br/scielo.php?pid=S1679-49742022000201700&script=sci_arttext
- López-Franco MD, Parra-Anguita L, Comino-Sanz IM,
Pancorbo-Hidalgo PL. Development and validation of the Pressure Injury
Prevention Barriers questionnaire in hospital nurses in Spain. BMJ Open.
2020,10:e041376. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7780508/
- Melnyk B, Fineout-Overholt E. Evidence-based
practice in nursing & healthcare: A guide to best practice. 5th ed.
Philadelphia: Wolters Kluwer; 2023.
- Aloweni F, Ang SY, Fook‐Chong S, Agus N, Yong P,
Goh MM, et al. A prediction tool for hospital‐acquired pressure ulcers
among surgical patients: Surgical pressure ulcer risk score. International
Wound J [Internet]. 2018 Oct 5;16(1):164–75. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949343/
- Bai DL, Liu TW, Chou HL, Hsu YL. Relationship
between a pressure redistributing foam mattress and pressure injuries: An
observational prospective cohort study. Jutai J, editor. Plos One. 2020
Nov 9;15(11):e0241276. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7652312/
- Bereded DT, Salih MH, Abebe
AE. Prevalence and risk factors of pressure ulcer in hospitalized adult
patients; a single center study from Ethiopia. BMC Res Notes. 2018;11.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267874/
- Brophy S, Moore Z, Patton D, O’Connor T, Avsar P.
What is the incidence of medical device-related pressure injuries in
adults within the acute hospital setting? A systematic review. J Tissue
Viability [Internet]. 2021 Mar 29; Disponível em: https://www.sciencedirect.com/science/article/pii/S0965206X21000334
- Chaboyer W, Bucknall T, Gillespie B, Thalib L,
McInnes E, Considine J, et al. Adherence to evidence-based pressure injury
prevention guidelines in routine clinical practice: a longitudinal study.
International Wound J. 2017 Jul 25;14(6):1290–8. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949936/
- Cortés OL, Salazar-Beltrán LD, Rojas-Castañeda
YA, Alvarado-Muriel PA, Serna-Restrepo A, Grinspun D. View of Use of
Hydrocolloid Dressings in Preventing Pressure Ulcers in High-risk
Patients: a Retrospective Cohort. Udea.edu.co. 2018 Feb 15; 36. Disponível
em: https://revistas.udea.edu.co/index.php/iee/article/view/331952/20787943
- Cox J, Edsberg LE, Koloms K, VanGilder CA.
Pressure injuries in critical care patients in US hospitals. J Wound,
Ostomy Continence Nurs. 2022 Jan;49(1):21–8. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9200225/
- Debon R, Fortes VLF, Rós ACR, Scaratti M. The
Nurses’ Viewpoint Regarding the Use of the braden Scale With the Elderly
Patient / A Visão de Enfermeiros Quanto a Aplicação da Escala de Braden no
Paciente Idoso. Rev Pesq: Cuidado é Fundamental Online. 2018 Jul
1;10(3):817. Disponível em: http://seer.unirio.br/cuidadofundamental/article/view/6210
- Díaz-Caro I, Gómez-Heras GS. Incidence of
hospital-acquired pressure ulcers in patients with “minimal risk”
according to the “Norton-MI” scale. Nardone B, editor. Plos One. 2020 Jan
8;15(1):e0227052. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6948734/
- Edsberg LE, Cox J, Koloms K, VanGilder-Freese CA.
Implementation of pressure injury prevention strategies in acute care. J
Wound, Ostomy Continence Nurs. 2022 May;49(3):211–9. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9093720/
- Farias APEC, Queiroz RB. Risk factors for the
development of pressure injury in the elderly: integrative review /
Fatores de risco para o desenvolvimento de lesão por pressão em idosos:
revisão integrativa. Rev Pesq Cuidado é Fundamental Online. 2022 Oct
4;14:1–8. Disponível em: http://seer.unirio.br/cuidadofundamental/article/view/11423
- Garcia EQM, Silva BT, Abreu DPG, Roque TS, Sousa
JIS, Ilha S. Nursing diagnosis in older adults at risk for pressure
injury. Rev Esc Enfermagem USP. 2021 Aug 20;55. Disponível em: https://www.scielo.br/j/reeusp/a/STzLfSBkZJXtRQxpkhP4fwR/?lang=en
- Ham WH, Schoonhoven L, Schuurmans MJ, Leenen LP.
Pressure ulcers in trauma patients with suspected spine injury: a
prospective cohort study with emphasis on device-related pressure ulcers.
International Wound J. 2016 Jan 14;14(1):104–11. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949823/
- Ho C, Jiang J, Eastwood CA, Wong H, Weaver B,
Quan H. Validation of two case definitions to identify pressure ulcers
using hospital administrative data. BMJ Open. 2017 Aug;7(8):e016438.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5629722/
- Hyun S, Vermillion B, Newton C, Fall M, Li X,
Kaewprag P, et al. Predictive Validity of the Braden Scale for Patients in
Intensive Care Units. American J Critical Care. 2013 Nov 1;22(6):514–20.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4042540/
- Jiang Q, Li X, Qu X, Liu Y, Zhang L, Su C, et al.
The incidence, risk factors and characteristics of pressure ulcers in
hospitalized patients in China. Inter jclinical experimental pathol
[Internet]. 2014; 7(5):2587–94. Disponível em:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069923/
- Jiang X, Hou X, Dong N, Deng H, Wang Y, Ling X,
et al. Skin temperature and vascular attributes as early warning signs of
pressure injury. J Tissue Viability. 2020 Nov;29(4):258–63. Disponível em:
https://www.sciencedirect.com/science/article/pii/S0965206X20301108?via%3Dihub
- Labeau SO, Afonso E, Benbenishty J, Blackwood B,
Boulanger C, Brett SJ, et al. Prevalence, associated factors and outcomes
of pressure injuries in adult intensive care unit patients: the DecubICUs
study. Intensive Care Medicine. 2020 Oct 9;47(2):160–9. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7880913
- Lee YJ, Kim JY, Dong CB, Park OK. Developing
risk-adjusted quality indicators for pressure ulcers in long-term care
hospitals in the Republic of Korea. International Wound J. 2019 Feb
22;16(1):43–50. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949183/
- Linnen DT, Kipnis P, Rondinelli J, Greene JD, Liu
V, Escobar GJ. Risk Adjustment for Hospital Characteristics Reduces
Unexplained Hospital Variation in Pressure Injury Risk. Nurse Res.
2018;67:314-323. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6023742/
- Liu Y, Wu X, Ma Y, Li Z, Cao J, Jiao J, et al.
The prevalence, incidence, and associated factors of pressure injuries
among immobile inpatients: A multicentre, cross‐sectional, exploratory
descriptive study in China. International Wound J. 2019 Jan
22;16(2):459–66. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949263/
- Lopes TF, Fernandes BKC, Alexandre SG, Farias FS,
Day TC, Freitas MC de. Medicines and its relation to the development of
pressure injury in hospitalized-elderly people / Medicamentos e sua
relação com o desenvolvimento de lesão por pressão em idosos
hospitalizados. Rev Pesq Cuidado é Fundamental Online [Internet]. 2020
[cited 2022 Jan 6];12:222–6. Disponível em: http://www.seer.unirio.br/cuidadofundamental/article/view/7993/pdf
- Mutair AA, Ambani Z, Obaidan FA, Salman KA,
Alhassan H, Mutairi AA. The effectiveness of pressure ulcer prevention
programme: A comparative study. International Wound Journal. 2019 Nov
6;17(1):214–9. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7948995/
- Oe M, Sasaki S, Shimura T, Takaki Y, Sanada H.
Effects of Multilayer Silicone Foam Dressings for the Prevention of
Pressure Ulcers in High-Risk Patients: A Randomized Clinical Trial.
Advances in Wound Care. 2020 Feb 4;9(12). Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7698645
- Padula WV, Gibbons RD, Valuck RJ, Makic MBF,
Mishra MK, Pronovost PJ, et al. Are Evidence-based Practices Associated
With Effective Prevention of Hospital-acquired Pressure Ulcers in US
Academic Medical Centers? Medical Care. 2016 May;54(5):512–8. Disponível
em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834884/
- Pickham D, Berte N, Pihulic M, Valdez A, Mayer B,
Desai M. Effect of a wearable patient sensor on care delivery for
preventing pressure injuries in acutely ill adults: A pragmatic randomized
clinical trial (LS-HAPI study). International J Nurs Studies. 2018
Apr;80:12–9. Disponível em: https://www.sciencedirect.com/science/article/pii/S0020748917302869?via%3Dihub
- Santamaria N, Gerdtz M, Sage S, McCann J, Freeman
A, Vassiliou T, et al. A randomized controlled trial of the effectiveness
of soft silicone multi-layered foam dressings in the prevention of sacral
and heel pressure ulcers in trauma and critically ill patients: the border
trial. International Wound J [Internet]. 2013 May 27;12(3):302–8.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950350/
- Serpa LF, Oliveira AS, Nogueira PC, Santos VLCG.
Risk for undernutrition and development of pressure injury in hospitalized
patients in Brazil: Multicentre prospective cohort study. Int Wound J.
2020;17:916-924. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7948825/
- Sousa I, Kapp S, Santamaria N. Positioning
immobile critically ill patients who are at risk of pressure injuries
using a purpose‐designed positioning device and usual care equipment: An
observational feasibility study. International Wound J. 2020 Apr
18;17(4):1028–38. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949009/
- Shaw LF, Chang PC, Lee JF, Kung HY, Tung TH.
Incidence and Predicted Risk Factors of Pressure Ulcers in Surgical
Patients: Experience at a Medical Center in Taipei, Taiwan. BioMed Res
International [Internet]. 2014 [cited 2019 Nov 21];2014:1–9. Disponível
em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4099038/
- Wang LH, Chen HL, Yan HY, Gao JH, Wang F, Ming Y,
et al. Inter-rater reliability of three most commonly used pressure ulcer
risk assessment scales in clinical practice. International Wound J. 2014
Sep 16;12(5):590–4. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950447/
- Yoshimura M, Ohura N, Tanaka J, Ichimura S,
Kasuya Y, Hotta O, et al. Soft silicone foam dressing is more effective
than polyurethane film dressing for preventing intraoperatively acquired
pressure ulcers in spinal surgery patients: the Border Operating room
Spinal Surgery (BOSS) trial in Japan. International Wound J. 2016 Dec
7;15(2):188–97. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950169/
- Yoshimura M, Ohura N, Santamaria N, Watanabe Y,
Akizuki T, Gefen A. High body mass index is a strong predictor of
intraoperative acquired pressure injury in spinal surgery patients when
prophylactic film dressings are applied: A retrospective analysis prior to
the BOSS Trial. International Wound J. 2020 Feb 17;17(3):660–9. Disponível
em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949170/
- Lovegrove J, Fulbrook P, Miles S. Prescription of
pressure injury preventative interventions following risk assessment: An
exploratory, descriptive study. International Wound J. 2018 Aug
2;15(6):985–92. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950082/
- Smith SK, Ashby SE, Thomas L, Williams F. Avaliação
de uma abordagem multifatorial para reduzir a prevalência de lesões por
pressão em ambientes regionais australianos de internação aguda. Int.
Wound J. 2017;15:95-105. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949924/
- Sternal D, Wilczyński K, Szewieczek J. Pressure
ulcers in palliative ward patients: hyponatremia and low blood pressure as
indicators of risk. Clinical Interventions in Aging. 2016 Dec; 12:37–44.
Disponível em:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207332/
- Schoeps LN, Tallberg AB, Gunningberg L. Patients’
knowledge of and participation in preventing pressure ulcers- an
intervention study. International Wound J. 2016 Apr 26;14(2):344–8.
Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950178/
- Cheng H, Sun X, Ji X, Zhang J, Lv J, Li T, et al.
Risk factors and the potential of nomogram for predicting
hospital‐acquired pressure injuries. International Wound Journal. 2020 Apr
7;17(4):974–86. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7949427/
- Song W, Kang M-J, Zhang L, Jung W, Song J, Bates
DW et al. Predicting pressure injury using nursing assessment phenotypes
and machine learning methods. J. Am. Med. Inform. Assoc.
2021;28:759-65. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7973453/
- Oh YS, Kim J-H, Xie Z, Cho S, Han H, Jeon SW et
al. Battery-free, wireless soft sensors for continuous multi-site
measurements of pressure and temperature from patients at risk for
pressure injuries. Nat Commun. 2021;12:e:5008. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8385057/
- Mehaffey JH, Politano AD, Bhamidipati CM, Tracci
MC, Cherry KJ, Kern JA, et al. Decubitus ulcers in patients undergoing
vascular operations do not influence mortality but affect resource
utilization. Surgery [Internet]. 2017 Jun 1 [cited 2023 Sep
28];161(6):1720–7. Disponível em https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433886/
- Silva CFR, Santana RF, Oliveira BGRB, Carmo TG.
High prevalence of skin and wound care of hospitalized elderly in Brazil:
a prospective observational study. BMC Res. Notes. 2017;10. Disponível em:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5290646/
Funding
and Acknowledgements:
We
inform that this research did not receive funding.
Authorship
criteria
We
inform that all the authors mentioned above contributed substantially to the
conception and planning of the study; to the collection, analysis and interpretation
of data; as well as to the writing, critical review and final approval of the
version sent to the Journal.
Declaration
of conflict of interest
Nothing
to declare.
Scientific Editor: Francisco Mayron
Morais Soares. Orcid: https://orcid.org/0000-0001-7316-2519
Rev Enferm Atual In Derme 2025;99(1): e025032