REVIEW ARTICLE
IDENTIFYING
CHECKLISTS TYPE INSTRUMENTS WITH A FOCUS ON SAFE VAGINAL BIRTH CARE
IDENTIFICAR LISTAS
DE VERIFICACIÓN DE INSTRUMENTOS CON UN ENFOQUE EN LA ATENCIÓN SEGURA DEL PARTO
VAGINAL
IDENTIFICANDO
INSTRUMENTOS TIPO CHECKLISTS COM ENFOQUE NOS
CUIDADOS AO PARTO VAGINAL SEGURO
https://doi.org/10.31011/reaid-2025-v.99-n.supl.1-art.2335
1Tamires Alves Dias
2Ana Karoline Alves
da Silva
3Simony de Freitas
Lavor
4Patrícia Pereira
Tavares de Alcântara
5Maria do Socorro
Vieira Lopes
6Rachel de Sá
Barreto Luna Callou Cruz
1Universidade Regional do Cariri – URCA,
Iguatu/CE, Brazl. ORCID: https://orcid.org/0000-0003-0420-0977.
2Universidade Regional do Cariri – URCA,
Iguatu/CE, Brazil. ORCID: https://orcid.org/0000-0003- 0686-1808
3Universidade Regional do Cariri – URCA,
Iguatu/CE, Brazil. ORCID: https://orcid.org/0000-0001- 8568-5501
4FIOCRUZ, Crato/CE, Brasil. ORCID: https://orcid.org/0000-0003-3337-4845
5Universidade Regional do Cariri – URCA,
Crato/CE, Brazil. ORCID: https://orcid.org/0000-0003-1335-5487
6Universidade Regional do Cariri – URCA,
Crato/CE, Brazil. ORCID: https://orcid.org/0000-0002-4596-313X
Corresponding Author
Tamires Alves Dias
Rua Eriton Barros
Costa, 174-C, Novo Iguatu, CEP: 63.504-775, Iguatu/CE – Brazil. Contact +55(88)
99628-6028. E-mail: alvestamires98@gmail.com
Submission: 24-07-2024
Approval: 30-04-2025
ABSTRACT
The objective was
to identify the existence of checklists available in the scientific literature
focusing care for safe vaginal birth. This is an integrative review, carried
out in January 2024, using the following databases: Latin American and
Caribbean Literature in Health Sciences (LILACS), Medical Literature Analysis
and Retrieval System Online (MEDLINE), Nursing Database (BDENF). The following
Health Sciences Descriptors (DeCS) were used: “Checklist”, “Normal childbirth”,
“Patient safety” and the use of Boolean connectors “AND”. The main information
contained in the six articles selected was then presented. The studies proved
to be relevant, pointing out that the use of the checklist stood out for being
a tool capable of pointing out the recommendations to be followed by professionals,
as well as providing women who received safe and quality care during labor.
However, no study was found that specifically presented data on the use of a
checklist, focusing on nursing care during safe vaginal delivery. This
highlights the social and scientific relevance of conducting new studies to
address this gap.
Keywords: Checklist; Normal
Childbirth; Patient Safety.
RESUMEN
El objetivo fue
identificar la existencia de listas de verificación disponibles en la
literatura científica enfocadas a la atención segura del parto vaginal. Se
trata de una revisión integradora, realizada en enero de 2024, a través de las
bases de datos: Literatura Latinoamericana y del Caribe en Ciencias de la Salud
(LILACS), Sistema de Análisis y Recuperación de Literatura Médica en Línea
(MEDLINE), Base de Datos en Enfermería (BDENF). Se utilizaron los Descriptores
de Ciencias de la Salud (DeCS): “Lista de Verificación”, “Parto Normal”,
“Seguridad del Paciente” y el uso de conectores booleanos “Y”. Posteriormente,
se expuso la información principal contenida en los seis artículos
seleccionados. Los estudios resultaron relevantes, señalando que el uso de la
lista de control se destacó por ser una herramienta capaz de señalar las
recomendaciones a seguir por los profesionales, así como por brindar a las
mujeres una atención segura y de calidad durante el parto. Sin embargo, se
destaca que no se encontró ningún estudio que presentara específicamente datos
sobre el uso de una lista de verificación, centrándose en los cuidados de
enfermería durante la asistencia al parto vaginal seguro. De esta manera, se
valora la relevancia social y científica de realizar nuevos estudios dirigidos
a esta brecha.
Palabras clave: Lista de
Verificación; Parto Normal; Seguridad del Paciente.
RESUMO
Objetivou-se
identificar a existência de checklists disponíveis na literatura
científica com enfoque nos cuidados ao parto vaginal seguro. Trata-se de uma
revisão integrativa, realizada em janeiro de 2024, por meio das bases de dados:
Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), Medical
Literature Analysis and Retrievel System Online (MEDLINE), Base de Dados
em Enfermagem (BDENF). Empregou-se os Descritores em Ciências da Saúde (DeCS):
“Checklist”, “Parto normal”, “Segurança do Paciente” e o uso de conectores booleanos
“AND”. Posteriormente, foram expostas as principais informações contidas nos
seis artigos selecionados. Os estudos demonstraram-se relevantes, ao apontar
que a utilização do checklist destacou-se por ser uma ferramenta capaz
de apontar as recomendações a serem seguidas pelos profissionais, como também,
por proporcionar às mulheres que receberam os cuidados seguros e de qualidade
durante do trabalho de parto. Contudo, ressalta-se que não foi encontrado
nenhum estudo que apresentasse especificamente dados sobre a utilização de um checklist, com enfoque
nos cuidados de Enfermagem durante
a assistência ao parto vaginal seguro. Desse modo, valoriza-se a
relevância social e científica da realização de novos estudos voltados a essa
lacuna.
Palavras-chave: Checklist; Parto Normal; Segurança do Paciente.
INTRODUCTION
The final
period of pregnancy and childbirth are processes marked by physical and
psychological changes, which in most cases require care and technologies that
minimize the risks of maternal and neonatal morbidity and mortality. The World
Health Organization(1) points out the importance of promoting safe
and qualified care during the pre-, intra- and postpartum periods. However, of
the more than 130 million births that occur annually in Brazil, approximately
303,000 result in the death of the mother and other aggravating factors(2).
Maternal
mortality (MM), which occurs during pregnancy or within 42 days after its end,
is a reflection of the access to and quality of health services in a country.
It can be classified as direct and indirect, resulting from obstetric
complications during pregnancy, childbirth and/or in the puerperium, resulting
from negligence or inadequate treatment, pre-existing or developed diseases, aggravated
by effects of the moment(3,4).
In this
context, attempts to improve health indicators, such as the Humanization
Program in Prenatal and Birth (PHPN) created in 2000, as well as the Stork
Network created in 2011, emerged with the purpose of reducing the high rates of
maternal and perinatal morbidity and mortality, in addition to the excessive
use of obstetric interventions without scientific basis(5,6).
However,
there is much to be done for women's rights, especially in ensuring a safe and
quality birth, including the need to create individualized instruments for
providing health care, specialized, comprehensive and humanized monitoring, in
addition to the creation of public policies. It is important to emphasize that
one of the factors that hinder this guarantee is the incorrect management of
good practices for vaginal birth(4,7).
It is
noted that between the years 2016 and 2021, the number of officially registered
maternal deaths was 11,444 women. The maternal mortality ratio (MMR), one of
the most important global health indicators, which refers to the number of
deaths due to causes related to pregnancy, childbirth and puerperium per
100,000 live births, shows that in 2021, there were 110 deaths, the same rate
as in 1998(2).
In view of
this, adequate and safe care at the time of childbirth is essential for women
to experience motherhood in the best possible way. To ensure safety and
well-being, it is essential that the health team is prepared and well-informed
to carry out procedures and deal with possible complications(8,9).
It is
timely to encourage the implementation of tools that guide improvements in the
quality of care offered by health professionals, in addition to strengthening
safety from admission to discharge, enabling the diagnosis of care failures and
the creation of barriers so that they do not occur again(10,11).
In order
to maximize the quality of childbirth care, the WHO (12) developed a
Checklist for safe childbirth to prevent the main global causes of maternal and
perinatal deaths due to intrapartum causes, including hemorrhages, infections,
hypertension and complications during birth. This international initiative
indicates four pause points at which “checks” should be made: 1. Upon
admission; 2. Before expulsion (or cesarean section); 3. Immediately after
birth (up to 1 hour); 4. Before discharge. However, it is important to note
that this instrument is not aimed at nursing(12).
Thus, the
importance that the use of technologies such as checklists can bring to care is
highlighted. They are a constituent element of the work process and can be
classified as soft, soft-hard and hard. All of them treat technology
comprehensively, through the analysis of the entire production process, up to
the final product. Soft technologies are those of relationships; the soft-hard
ones are those of structured knowledge, such as theories, and the hard ones are
those of material resources(13).
Therefore,
taking into account the recommendations of the Guide for the implementation of
the WHO Safe Childbirth Checklist, together with information recommended by the
National Guidelines for Care in Normal Childbirth of the Ministry of Health
(MS) and other scientific evidence, the proposal for the construction and
validation of a soft-hard technology instrument is presented: a checklist(1,8,14).
Checklists
are structured tools that have several items or actions to be considered and/or
performed to confirm, through systematic observation, whether the necessary
activities and interventions are being implemented during their execution.
These have been adopted in a wide variety of environments and represent
promising strategies for a culture of patient safety, associated with greater
detection of potential risks during care(15,16).
In the
health area, the use of checklists contributes to the management,
systematization and application of care technologies. However, checklists are
not capable of solving all problems; however, they help maintain habits aimed
at the co-accountability of all members of the work team and measures such as
standardization and double checking(8,17).
Technology
in the care offered during vaginal delivery can be related to the development
of safe and non-invasive practices. In this context, their use allows the
promotion of humanization of care during labor and birth, respecting women in
their entirety and strengthening safety(11).
In view of
the above, it is clear that there is a need to conduct a review so that the
checklist can be constructed based on what is described and evidenced in the
literature, in order to support evidence-based care.
This study
may support contributions to the 3rd target of the Sustainable Development
Goals (SDGs), which aims to ensure a healthy life and promote well-being for
all, at all ages, thus achieving a reduction in the global maternal mortality
rate by 2030.
It also
has social and scientific-academic relevance in the healthcare field. It is
considered that the participation of nursing professionals may support the
recognition and greater reporting of cases of care failures and the creation of
barriers, allowing the competent bodies to have access to information and
develop public policies, contributing to the recognition of evidence-based
practices and adding quality of life to women.
Therefore, the objective was to identify the existence of checklists
available in the scientific literature focusing on care for safe vaginal birth.
METHOD
The study is an Integrative
Review, which consists of a method that seeks to synthesize the results through
conducting research on a given topic, in a systematic and comprehensive manner,
which facilitates access to in-depth information on the subject(18).
The content was produced by
conducting a bibliographic review of the Integrative Review type of literature,
according to the steps proposed by authors(18): 1) Definition of the
review question; 2) Search and selection of primary studies; 3) Extraction of
data from primary studies; 4) Critical evaluation of primary studies; 5)
Synthesis of results; 6) Presentation of the review(18).
The PVO strategy was used
to develop the guiding question (P - population; V - variable(s); O - outcome),
which corresponds to an acronym used to create the search strategy, which is
presented in Table 1.
Table 1 - PVO strategy for developing the guiding question. Crato, Ceará,
Brazil, 2024.
|
ESTRATEGY
|
DESCRIPTION
|
DESC
|
|
Population (P)
|
Nursing Care
|
Checklist
|
|
Variables (V)
|
Intrapartum care actions
|
Regular birth
|
|
Expected outcomes(O)
|
Guarantee of safe childbirth
|
Patient safety
|
Source: Prepared by
the author.
By implementing the PVO
acronym, the following guiding question was raised: Are there checklists
available in the scientific literature focusing on nursing care for safe
vaginal delivery?
The
process of searching and selecting studies took place during the month of
January 2024 through the following databases: Latin American and Caribbean
Literature in Health Sciences (LILACS), Medical Literature Analysis and
Retrieval System Online (MEDLINE), and Nursing Database (BDENF). The following
Health Sciences Descriptors (DeCS) were used: “Checklist”, “Normal Delivery”,
“Patient Safety” and the use of Boolean connectors “AND” (Table 2).
Table 2 - Search strategy used in the databases. Crato, Ceará, Brazil,
2024.
|
DATABASE
|
DECS
|
|
MEDLINE
|
1.
Checklist AND Regular birth
2.
Regular birth
AND Patient Safety
|
|
LILACS
|
1.
Checklist AND Regular birth
2.
Regular birth
AND Patient Safety
|
|
BDENF
|
1.
Checklist AND Regular birth
2.
Regular birthAND
Regular birth
|
Source: Prepared by
the author.
The inclusion criteria were: original articles, in
full, in Portuguese, English and Spanish. The exclusion criteria were:
duplicated studies, incomplete studies, course completion studies and
literature reviews. A time frame of the last five years was used.
For
the study selection process, an adaptation of a flowchart called PRISMA
(Preferred Reporting Items for Systematic reviews and Meta-Analyses)(19) was
used, and is presented below in Figure 1.
Figure 1 – Flowchart of the selection of studies
included in the review. Crato, Ceará, Brazil, 2024.
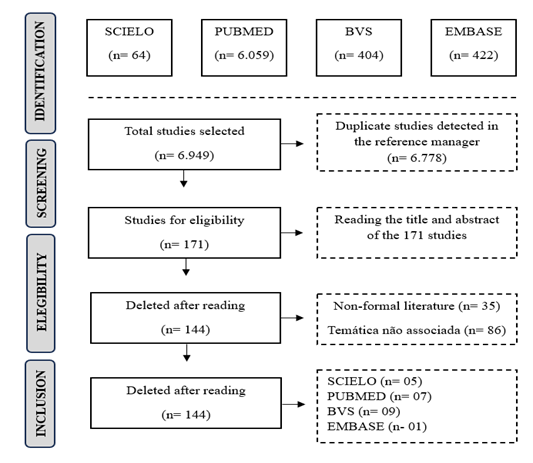
 Source: Adapted from PRISMA-ScR (2009).
Source: Adapted from PRISMA-ScR (2009).
For the
data extraction process, an adapted form was used, which allows each article to
be analyzed separately in order to identify the main information contained in
the text. This instrument includes the following items: identification of the
article (title, year of publication, country); objective; methodological
characteristics (type of publication); level of evidence; main results and
conclusion.
The
studies were evaluated and categorized based on the levels and quality of
evidence described in seven levels, a modification of the Agency for Health
care Research and Quality (AHRQ).
The
division is presented as follows: Level 1 (systematic review or meta-analysis
of randomized controlled clinical trials or from clinical guidelines based on
systematic reviews of randomized controlled clinical trials); Level 2
(well-designed randomized controlled clinical trial); Level 3 (well-designed
clinical trials without randomization); Level 4 (well-designed cross-sectional,
cohort and case-control studies); Level 5 (systematic review of descriptive and
qualitative studies); Level 6 (a single descriptive or qualitative study) and
Level 7 (opinion of authorities and/or report of expert committees)(20).
The data
obtained were organized in a spreadsheet in Microsoft Windows Word, version
2019, using the data reduction method, which consists of performing a thorough
reading and applying classification techniques.
At this stage, the results and their interpretation were organized
in a table, in order to facilitate visualization and, consequently, the
interpretation of the findings. Subsequently, a discussion was prepared with
the scientific findings on the topic.
RESULTS
The characterization of the
six studies included, including the title, country, year of publication, type
of study, database in which the study was inserted, and the level of scientific
evidence (LE) is shown in Table 3.
Table 3 -
Characterization of the studies included in the Review. Crato, Ceará, Brazil,
2024.
|
Order
|
Title
|
Country/ Year
|
Type of study
|
N.E
|
Database
|
|
A121
|
Checklist: A useful and safe tool for initiating care for eutocic
vaginal delivery
|
Spain 2021
|
Descriptive
observational study
|
N6
|
MEDLINE
|
|
A222
|
Society
for Maternal Fetal Medicine: Postpartum Visit Checklists for Normal and
Complicated Pregnancy
|
USA
2022
|
Descriptive
study
|
N6
|
MEDLINE
|
|
A323
|
Improving
maternal health and safety through adherence to the postpartum hemorrhage
protocol in Latin America
|
Peru
2014
|
Multicenter descriptive study
|
N5
|
LILACS
|
|
A424
|
Checklist
on intrapartum care
in
normal birth
|
Brazil 2021
|
Cross-sectional
study
|
N4
|
BDENF
|
|
A525
|
Subpopulation Analysis with Principles of the BetterBirth Study
and the Impact of the WHO Safe Childbirth Checklist Intervention
|
Kenya
2022
|
Study
prognosis
|
N5
|
MEDLINE
|
|
A626
|
Nursing professionals' perception of the use of the safe
childbirth checklist
|
Brazil
2021
|
Qualitative
study
|
N5
|
BDENF
|
Source: Prepared by
the author.
The six
selected studies were published between 2014 and 2022, with one published in
2014 (16%), two in 2022 (32%) and three in 2021 (52%), representing a slight
predominance in 2021.
These
studies are indexed in international databases, namely: Medical Literature
Analysis and Retrieval System Online (MEDLINE); Nursing Database (BDENF) and
Latin American Literature in Health Sciences (LILACS).
The studies were identified by abbreviations and numbering from A1
to A6. The objectives and main results are presented below in Table 4.
Table 4 – Summary of objectives and main
results obtained from the included studies. Crato, Ceará, Brazil, 2024.
|
Order
|
Objective
|
Main results
|
|
A121
|
Assess the degree of
compliance with each item that constitutes the checklist tool after having
assisted between 25 and 30 vaginal births
|
The importance of using a
checklist to anticipate risk situations and reduce the number of adverse
perinatal outcomes was identified, and it would be interesting to have a
tool, such as the proposed checklist, that facilitates the learning process
and the adequate progress of participants.
|
|
A222
|
Facilitate completion of all key components
of postpartum care and provide a safe and effective transition to healthy
care
|
The postpartum checklists
facilitated completion of all key components of postpartum care and provided
a safe and effective transition to healthy care. The checklists were also
found to facilitate targeting of additional counseling and referral needs for
patients with underlying chronic conditions or who had pregnancy
complications, proving to be a useful tool
|
|
A323
|
Determine provider
compliance with protocols for preventing postpartum hemorrhage
|
It was possible to see that through
training in adherence to postpartum hemorrhage prevention protocols, there
was a significant improvement in the safety of parturients.
|
|
A424
|
Apply the intrapartum care checklist for
vaginal delivery
|
It was observed that the
professionals obtained a good adherence rate in relation to the practices
evaluated in the checklist, always seeking ways to reduce harm related to
childbirth. Furthermore, it was shown that the births assisted by these
professionals have fewer interventions and were permeated by good practices.
|
|
A525
|
Identify subpopulations with divergent
characteristics that benefited from the checklist intervention with
significantly reduced risks of deaths and complications
|
A Lista de Verificação do
Parto Insurance resulted in improvements in maternal and neonatal health care
and outcomes. Mother-infant dyads were found to benefit from the Checklist
intervention, resulting in 2.6% neonatal death in the intervention arm
compared with 3.66% in the control arm
|
|
A626
|
Understand how the implementation of the Safe
Birth Checklist changed obstetric practice
|
The professionals understood that
the instrument brought benefits and contributed to greater quality and safety
in obstetric care, in addition to encouraging a culture of safety.
|
Source: Prepared by
the author.
DISCUSSION
It is
important to note that no study was found in the literature that specifically
presented data on the use of a checklist in the results, focusing on nursing
care during safe vaginal delivery. However, the study (24) indicates
that nursing is the predominant professional category in relation to care and
monitoring during labor.
It is
important to emphasize the importance that these professionals bring to the
care and comfort of the parturient during labor. Regarding the focus on nursing
care for safe vaginal delivery, the study (24) highlighted the
adherence rate of some practices, such as the professional performing a vaginal
examination every four hours, the use of uterotonics only when necessary,
encouraging vertical delivery and reducing obstetric violence.
In recent
years, nursing has gained space in public health policies due to its qualified
and humanized view of the birth process, applying efforts to ensure that it
flows naturally without the need for unnecessary interventions (9).
Nursing
care requires constant records of routine procedures in the work process. Thus,
the checklist represents another means of transferring information and
interaction, but also a way of organizing care. Thus, a study(26) reinforces
that the checklist is part of the systematization of nursing care, which allows
for the reduction of adverse events in the care provided and, consequently,
improvement in the quality of care.
Benefits
arising from the use of the checklist to guide care were evident: they
perceived greater attention in identifying failures and weaknesses in the care
of the parturient; they saw in the checklist the possibility of avoiding
forgetfulness; they mentioned the importance of the checklist phases, a
standardized direction in care, greater interaction and better communication
between team members(26).
It was
identified that the checklist is of utmost importance, as it identifies that
patient safety is directly related to the procedure, in relation to the absence
of damage or accidents of injuries during the provision of health care; given
the reduction of errors in the health area. In more recent research, it was
found that professionals exposed to stressful and complex conditions should use
tools that give them security and assertiveness, and that these tools are
simple, allowing them to comply with procedures without errors (16).
Similarly, studies have indicated that the use of checklists
improved communication and interprofessional relationships and the direction of
actions, given that they gather fundamental information that is quick and easy
to apply. A Brazilian study indicated that the checklist is an easy-to-apply
instrument that facilitates the work routine from the professional's
perspective and helps to avoid forgetting and speed up the approach to a large
number of factors related to the client's context (26).
The WHO(1)
made recommendations regarding natural childbirth care, in the sense that
institutions and professionals who provide childbirth care aim to respect and
provide dignity to the woman in labor, the newborn and family members, through
changes in paradigms, protocols and attitudes to provide an active and healthy
natural childbirth. Thus, when effectively instituted, through protocols,
standards or routines, encouraging the use of a checklist favors safety and
humanized care(1).
However,
authors(25) emphasize that the WHO Safe Childbirth Checklist does
not encompass the reality of all services in the country, which reinforces the
indispensability of creating and using other technologies that assist in the
stages of care during vaginal childbirth.
Corroborating
this, a study(7) indicates that the use of a checklist can provide
nurses with an approach based on the Systematization of Nursing Care (SAE),
linking better planning, effective interventions and the achievement of a
prognosis for users admitted in labor until their discharge from the
institution.
It is
evident that nursing care is associated with better results in labor and
delivery, reducing unnecessary interventions, including cesarean sections,
increasing women's satisfaction with the care received and presenting better
perinatal results.
Studies indicate that women during labor and vaginal delivery
assisted by obstetric nurses had more access to good practices recommended by
the WHO and the Ministry of Health (MS) than when assisted in the traditional
model without the presence of this professional (9).
The use of a checklist is an important tool, as it can
present recommendations to be followed by professionals, as well as provide
women who have received safe and quality care during labor. The results of the
review indicate the importance of using a checklist in providing care for safe
vaginal delivery.
The checklist can be a low-cost, practical and
easy-to-understand and complete option for professionals to use. In addition,
it can contribute to the listing of evidence-based recommendations during
labor, demonstrating that professionals can provide less interventionist, more
respectful care within the ethical criteria of autonomy, maintaining or
improving perinatal outcomes, benefiting safe and quality care.
However,
it is noteworthy that no study was found that specifically presented data on
the use of a checklist, focusing on nursing care during safe vaginal delivery.
Thus, the social and scientific relevance of conducting new studies aimed at
filling this gap is valued.
1.
Organização
Mundial de Saúde. Guia de Implementação da Lista de Verificação da OMS para Partos Seguros: melhorar a qualidade dos partos realizados em unidades de saúde para as mães e os recém-nascidos. Genebra:
OMS; 2017.
2.
Observatório
Obstétrico Brasileiro. Razão de morte materna
brasileira. Levantamento estatístico. Observatório Obstétrico Brasileiro (OOBr); 2022.
3. Ranzani OT, Marinho
MF, Bierrenbach AL. Utilidade do Sistema de Informação Hospitalar da mortalidade materna
no Brasil. Rev Bras Epidemiol. 2023;26(230007):1-9.
4. Ferreira MES, Coutinho
RZ, Queiroz BL. Morbimortalidade materna
no Brasil e a urgência de um sistema de vigilância do near miss materno.
Cad. Saúde Pública. 2023;39(8)1-13.
5.
Rodrigues
MS. Humanização no processo de parto e nascimento: implicações do plano
de parto [dissertação]. Belo Horizonte (MG): Universidade Federal de Minas Gerais; 2017.
6. Flores TR, Neves RG, Mielke GI, Bertoldi AD, Nunes BP. Desigualdades na cobertura da assistência pré-natal
no Brasil: um estudo de abrangência nacional. Cien
Saúde Colet. 2021;26(2):593-600.
7.
Nascimento ER, Santos ECS, Sousa DS, Gallotti FCM. Desafios
da assistência de enfermagem ao parto humanizado. Cad Grad Ciên Biol Saúde UNIT.
2020;6(1):141-46.
8. Ministério da Saúde (BR). Nota técnica para organização da rede de
atenção à saúde com foco na atenção primária à saúde e na atenção ambulatorial
especializada – saúde da mulher na gestação, parto e puerpério. Brasília (DF):
Ministério da Saúde; 2019.
9. Monteiro AMS. A Assistência de Enfermagem Obstétrica no Trabalho de Parto.
Rev Paul Enferm. 2022;33(1):1-12.
10.
Cunha EML. Implantação do checklist do parto seguro
[trabalho de conclusão de curso]. Teresina (PI): Universidade Federal do Piauí;
2018.
11.
Duarte MR, Alves VH, Rodrigues DP, Souza KV,
Pereira AV, Pimentel MM. Tecnologias do cuidado na enfermagem obstétrica:
contribuição para o parto e nascimento. Cogit Enferm. 2019;24(54164):1-11.
12.
Organização Mundial de Saúde. Lista de Verificação
para Partos Seguros. Genebra: OMS; 2015.
13.
Merhy EE, Chakkour M, Stéfano E, Stéfano ME, Santos
CM, Rodrigues RA. Em busca de ferramentas analisadoras das tecnologias em
saúde: a informação e o dia a dia de um serviço, interrogando e gerindo
trabalho em saúde. In: Merhy EE, Onocko R, organizadores. Agir em saúde: um
desafio para o público. São Paulo: Hucitec; 2006. p. 113-50.
14.
Teles LMR. Construção e validação de tecnologia
educativa para acompanhantes durante o trabalho de parto [dissertação].
Fortaleza (CE): Universidade Federal do Ceará; 2011.
15.
Maran E, Matsuda LM, Marcon SS, Haddad MCFL, Costa
MAR, Magalhães AMM. Adaptação e validação de Checklist Multidisciplinar para
rounds em Unidade de Terapia Intensiva. Texto Contexto Enferm.
2022;31(20210047):1-13.
16.
Trindade AO, Paiva FMF, Cardoso VNS. A relevância
da enfermagem na implantação do checklist em cirurgia pediátrica. Repositório
Universitário da Ânima; 2022.
17.
Franco RS, Franco CAGS. Avaliação com o uso de
Checklists e Escalas de Avaliação Global. In: Pereira Junior GA, Guedes HTV,
organizadores. Simulação em saúde para ensino e avaliação. 1° ed. São Carlos,
SP: Cubo Multimídia; 2021. p. 197-204.
18.
Mendes KDS, Silveira RCCP, Galvão CM. Uso de
gerenciador de referências bibliográficas na seleção dos estudos primários em
revisão integrativa. Texto Contexto Enferm. 2019;29(e20170204):1-13.
19.
Moher D, Liberati A, Tetzlaff J, Altman DG. Itens
de relatório preferidos para revisões sistemáticas e meta-análises: a
declaração PRISMA. PLoS Med. 2009;6(7):e1000097.
20.
Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan
B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing
service. Appl Nurs Res. 1998;11(4):195-206.
21.
Munõz MF, Angullo ZRR, Ricarte PP, Soto LC, Labarta
JR, Hernandéz IC, et al. Checklist: A Useful and Safe Tool for the Initiation
of Care for Eutocical Vaginal Delivery. Int. J. Environ. Res. Public Health.
2022;19(20):13409.
22.
Morgan J, Bauer S, Whitsel A, Combs CA. Postpartum
visit checklists for normal pregnancy and complicated pregnancy. Society for Maternal-Fetal
Medicine (SMFM). 2022;227(4):1-8.
23.
Olmedo B, Miranda E, Cordão O, Pettker CM, Funai
EF. Improving maternal health and safety through adherence to postpartum
hemorrhage protocol. Int J G Obstet. 2014;125(2):162-65.
24.
Carvalho LS, Rebouças BDS, Sousa LS, Ferreira
Junior AR, Carvalho REFL. Aplicação de checklist sobre cuidados intraparto no
parto normal. Rev Enferm Atual In Derme. 2021;95.
25.
Tadesse GA, Delaney MM, Akinwande V, Ogallo W,
Mershon CH, SemrauKE, et al. Principled subpopulation analysis of the
BetterBirth study and the impact of WHO's Safe Childbirth Checklist
intervention. AMIA Annu Symp Proc. 2022:1042-1051.
26.
Custódio RJM, Kapassi LB, Alves DT, Barros AF, Melo
MC, Boeckmann LMM, et al. Percepção dos profissionais de enfermagem sobre a utilização
do checklist do parto seguro. Cogitare Enferm. 2021;26(74752):1-10.
Funding and Acknowledgements:
The authors declare that the research did not
receive funding.
Authorship criteria (authors'
contributions)
The designation of authorship should be based
on the deliberations of the ICMJE, which considers an author as someone who:
1. contributes substantially to the conception
and/or planning of the study: Dias TA
2. in obtaining, analyzing and/or interpreting
the data: Dias TA; Cruz RSBLC.
3. as well as in the writing and/or critical
review and final approval of the published version: Dias TA; Alcântara PPT;
Silva AKA; Lavor SF; Lopes MSV; Cruz RSBLC.
Declaration
of conflict of interests
Nothing
to declare.
Scientific
Editor: Ítalo Arão
Pereira Ribeiro. Orcid: https://orcid.org/0000-0003-0778-1447
Rev
Enferm Atual In Derme 2025;99(supl.1): e025082
Source: Adapted from PRISMA-ScR (2009).