ORIGINAL ARTICLE
MEDICAL DEVICE-RELATED SKIN INJURIES IN NEONATES: A CROSS-SECTIONAL STUDY
LESIONES CUTÁNEAS ASOCIADAS A DISPOSITIVOS MÉDICOS EN NEONATOS: UN ESTUDIO TRANSVERSAL
LESÕES DE PELE ASSOCIADAS A DISPOSITIVOS MÉDICOS EM NEONATOS: ESTUDO TRANSVERSAL
https://doi.org/10.31011/reaid-2026-v.100-n.1-art.2695
1Carolina Tenfen
2Ivaneliza Simionato de Assis
3Geisyelli Alderete
4Marcos Augusto Moraes Arcoverde
5Bruno Taiki Takahasi
6Maria Fernanda Munhak da Silva
7Rosane Meire Munhak da Silva
1Hospital Universitário do Oeste do Paraná-HUOP, Cascavel – PR – Brazil. Orcid: https://orcid.org/0000-0002-6501-0248
2Centro Universitário Dinâmica das Cataratas-UDC, Foz do Iguaçu – PR – Brazil. Orcid: https://orcid.org/0000-0003-1166-6644
3Universidade Estadual do Oeste do Paraná-UNIOESTE, Foz do Iguaçu – PR – Brazil. Orcid: https://orcid.org/0000-0002-1609-8714
4Universidade Estadual do Oeste do Paraná-UNIOESTE, Foz do Iguaçu – PR – Brazil. Orcid: https://orcid.org/0000-0001-5104-559X
5Universidade Estadual do Oeste do Paraná-UNIOESTE, Cascavel – PR – Brazil. Orcid: https://orcid.org/0009-0002-1664-361X
6 Universidade Estadual do Oeste do Paraná-UNIOESTE, Cascavel – PR – Brazil. Orcid: https://orcid.org/0000-0001-6585-788X
7 Universidade Estadual do Oeste do Paraná-UNIOESTE, Foz do Iguaçu – PR – Brazil. Orcid: https://orcid.org/0000-0003-3355-0132
Autor correspondente
Ivaneliza Simionato de Assis
Avenida Tancredo Neves n. 5057, Bairro Porto Belo. Foz do Iguaçu- PR. Brazil. CEP: 85.867-633. phone: +55 (45) 984317395. E-mail: ivaneliza.assis@hotmail.com
Submission: 18-06-2025
Approval: 29-10-2025
ABSTRACT
Introduction: Skin injuries associated with the use of medical devices in neonates admitted to intensive care units represent a significant clinical challenge, especially among preterm infants and those with prolonged hospital stays. These injuries can impair skin integrity, increase infection risk, and extend hospitalization time. Objective: To analyze skin injuries in critically ill newborns related to the use of medical devices and describe the treatments employed. Methods: This cross-sectional epidemiological study was conducted in the neonatal intensive care unit of a university hospital in western Paraná, Brazil, between October 2022 and October 2023. Statistical analysis included the chi-square test, ANOVA, and Multiple Correspondence Analysis (p < 0,05). Results: The prevalence of skin injuries caused by medical devices was 29.46%, particularly in newborns with prolonged hospitalization. Nasal septum and occipital region injuries were the most common, caused by nasal prongs and inappropriate materials or inadequate repositioning, respectively. Device-related injuries were associated with a gestational age of less than 31 weeks (>60%), low birth weight (57%), and hospitalization exceeding 30 days (48.2%). Treatments included laser therapy (28.21%) for nasal septum injuries and polyurethane foam dressings (23.08%) for occipital region protection. Conclusion: Pressure injuries caused by medical devices can be prevented through measures such as selecting appropriate sites for devices, choosing less harmful materials, and training the multidisciplinary team.
Keywords: Newborn; Preterm; Injuries; Skin; Equipment and Supplies.
RESUMO
Introdução: As lesões de pele associadas ao uso de dispositivos médicos em recém-nascidos internados em unidades de terapia intensiva representam um importante desafio clínico, especialmente entre os prematuros e aqueles com longas internações. Essas lesões podem comprometer a integridade cutânea, aumentar o risco de infecções e prolongar o tempo de hospitalização. Objetivo: Analisar as lesões de pele em recém-nascidos críticos relacionadas ao uso de dispositivos médicos e descrever os tratamentos empregados. Métodos: Estudo epidemiológico, transversal, realizado em unidade de terapia intensiva neonatal de um hospital universitário do oeste do Paraná, Brasil, entre outubro/2022 e outubro/2023. A análise estatística incluiu teste qui-quadrado, ANOVA e Análise de Correspondência Múltipla (p < 0,05). Resultados: A prevalência de lesões de pele causadas por dispositivos hospitalares foi 29,46%, em especial para recém-nascidos com longo período de hospitalização. As lesões de septo nasal e em região occipital foram as mais prevalentes, causadas pelo uso de pronga nasal e material inadequado/mudança de decúbito frágil, respectivamente. As lesões por uso de dispositivos foram associadas a idade gestacional inferior a 31 semanas (>60%), baixo peso ao nascer (57%) e 30 dias de hospitalização (48,2%). Para o tratamento das lesões utilizou-se laserterapia (28,21%) em septo nasal e placa de poliuretano (23,08%) para proteção da região occipital. Conclusão: As Lesões por Pressão causadas pelo uso de dispositivos podem ser evitadas por medidas preventivas como a escolha do local apropriado para os aparelhos, pela escolha de materiais menos danosos e capacitação da equipe multiprofissional.
Palavras-chave: Recém-Nascido; Pré-Termo; Ferimentos; Pele; Equipamentos e Provisões.
RESUMEN
Introducción: Lesiones cutáneas asociadas al uso de dispositivos médicos en recién nacidos internados en unidades de cuidados intensivos representan un importante desafío clínico, especialmente entre los prematuros y aquellos con estancias hospitalarias prolongadas. Estas lesiones pueden comprometer la integridad cutánea, aumentar el riesgo de infecciones y prolongar el tiempo de hospitalización. Objetivo: Analizar las lesiones cutáneas en recién nacidos críticos relacionadas con el uso de dispositivos médicos y describir los tratamientos empleados. Métodos: Estudio epidemiológico, transversal, realizado en una unidad de cuidados intensivos neonatales de un hospital universitario del oeste de Paraná, Brasil, entre octubre de 2022 y octubre de 2023. El análisis estadístico incluyó prueba de chi-cuadrado, ANOVA y Análisis de Correspondencia Múltiple (p < 0,05). Resultados: La prevalencia de lesiones cutáneas causadas por dispositivos hospitalarios fue del 29,46%, especialmente en recién nacidos con estancias hospitalarias prolongadas. Lesiones en el tabique nasal y en la región occipital fueron las más prevalentes, causadas por el uso de cánula nasal y materiales inadecuados o cambios de decúbito deficientes, respectivamente. Las lesiones por dispositivos se asociaron con edad gestacional inferior a 31 semanas (>60%), bajo peso al nacer (57%) y 30 días de hospitalización (48,2%). Para el tratamiento se utilizó la laserterapia (28,21%) en el tabique nasal y la placa de poliuretano (23,08%) para proteger la región occipital. Conclusión: Lesiones por presión causadas por el uso de dispositivos pueden prevenirse mediante medidas como la elección adecuada del lugar de colocación, el uso de materiales menos agresivos y la capacitación del equipo multiprofesional.
Palabras clave: Recién Nacido; Prematuro; Lesiones; Piel; Equipos y Suministros.
INTRODUCTION
Prematurity represents a global public health problem, as it is considered the leading cause of infant mortality among children under five years of age and is responsible for half of the cases of neurological disorders in early childhood. Thus, the impact caused by premature birth affects not only the children, but also their caregivers, the health system, and society in general.(1)
The critical health conditions of many premature newborns demand intensive care with technological support and constant monitoring by medical devices, which are vital for their survival. However, this care involves invasive procedures that can lead to adverse events, compromising the integrity of these newborns' skin.(2)
The skin of a premature newborn is extremely fragile due to structural, cellular, and physiological immaturity. It is thinner, which reduces its mechanical resistance. Furthermore, it presents a loose connection between the epidermis and the dermis, making it susceptible to ruptures and lesions when subjected to pressure. This vulnerability is even more critical in newborns admitted to the Neonatal Intensive Care Unit (NICU).(3)
Prevention and management of skin lesions in hospitalized newborns are challenging due to the high incidence in NICUs and the difficulty of accessing less harmful devices. The main devices used include endotracheal tubes, nasal cannulas, ventilation masks, probes, catheters, sensors, diapers, drains, and fixation adhesives, which can compromise the newborn's skin when used improperly.(4)
One study demonstrated that medical devices were responsible for 31.3% of changes in the skin condition of hospitalized newborns.(2) It is also noteworthy that multiple types of skin lesions can occur in critically ill newborns, significantly contributing to increased hospitalization time.(5)
An international investigation into skin lesions in NICUs, focused mainly on premature newborns, revealed that 38% of lesions are associated with the use of medical and hospital devices.(6) The French Neonatal Society highlighted concerns about the high incidence of skin lesions in premature infants, especially on the face, resulting from the use of ventilatory support, which motivated them to seek strategies to reduce these rates.(7) In addition, a study conducted in Italy identified that 70% of Newborns developed at least one skin lesion.(8)
Skin lesions associated with devices, known as Pressure Injuries (PIs), can cause serious complications such as tissue necrosis and functional impairment. Furthermore, they increase the risk of secondary infections and sepsis, which prolongs hospital stay and increases hospital costs. These complications negatively impact the newborn's development, impairing both immediate recovery and long-term growth.(9)
The combination of fragile skin and the need for continuous support limits intervention options, as available products are often not ideal for premature newborns. Furthermore, the lack of suitable devices and difficulties in implementing effective measures exacerbate the challenge of efficiently managing this problem in neonatal units.(10)
Prevention strategies based on evidence-based clinical practices for newborn skin care include daily hygiene care, use of hydrocolloids on bony prominences, application of mineral oil for adhesive removal, and skin protection and cleansing measures.(11) The creation or implementation of scales and instruments for assessing skin lesions is also recommended, as well as professional training to reduce risk factors, promoting a safer and more effective approach.(12)
Given the above, it is essential to encourage new research exploring technological innovations aimed at the skin care of critically ill hospitalized newborns. These innovations, coupled with improvements in clinical practices, have the potential to reduce the incidence of skin lesions in neonatology, as well as improve health outcomes and quality of life for these vulnerable patients. In this context, this study aims to analyze skin lesions in critically ill newborns related to the use of medical devices and describe the treatments employed.
METHODS
This is a cross-sectional epidemiological study, developed based on the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline for scientific writing for observational studies.
The study was conducted in a NICU of a university hospital located in the western region of the state of Paraná, Brazil. The unit has ten beds structured to care for critically ill newborns from municipalities belonging to the tenth health region of the state. Most of the admitted newborns come from the Obstetric Center, the Neonatal Intermediate Care Unit of the institution itself, or from less complex hospitals.
Newborns hospitalized in the neonatal unit between October 2022 and October 2023 participated in the study, meeting the following inclusion criteria: newborns of any gestational age and/or with a diagnosis requiring hospitalization, and a score equal to or greater than 5 on the Newborn Skin Condition Scale (NSCS). Newborns with skin lesions unrelated to medical/hospital devices, those transferred to another NICU before the end of lesion treatment, and those who remained hospitalized after the end of data collection were excluded.
Data collection was performed by a neonatology resident nurse, previously trained by the principal investigator, who has extensive expertise in neonatal health research. Information was obtained through the analysis of electronic medical records in the Tasy® system.
A structured instrument was used for data
collection, including the independent variables: use of medical/hospital
devices and non-use of devices; and the dependent variables: i) Birth data:
sex, birth weight, gestational age, Apgar scores at one and five minutes; ii)
Hospitalization data: date of hospitalization, date of discharge or death; iii)
Initial lesion data: days of life at lesion appearance, lesion location, ECPRN
score, lesion origin, Neonatal Infant Pain Scale (NIPS) score; (12)
iiii) Injury evolution: treatment used, whether the injury worsened.
Data were coded in an Excel® spreadsheet by independent double
entry, followed by verification of inconsistencies. For analysis, the studied
variables were organized into double-entry tables and absolute and relative
frequencies were calculated.
To verify the relationship between the use of medical devices, the location of the injury, and the characteristics of the newborns, the chi-square test (Χ²) was applied. Furthermore, to compare the characteristics of newborns with injuries caused by medical devices, categorized according to the location of the injury (head/neck, limbs, and thorax/abdomen), a statistical analysis was performed in which continuous variables were described by means and standard deviations (SD). Differences between groups were evaluated using the ANOVA (Analysis of Variance) test. Both tests adopted a significance level of 0.05.
The identification of association patterns between categorical variables and the graphical representation of relationships between different groups and categories were performed using Multiple Correspondence Analysis (MCA). This technique was employed to explore the interactions between the clinical characteristics of newborns and the locations of lesions (such as head/neck, limbs, and thorax/abdomen), offering a comprehensive view of the associations present in the dataset. All statistical analyses were performed using Jamovi 2.3.28 software.
The research received approval from the University's Research Ethics Committee, opinion number 5,656,829 in 2022, and complied with Resolution No. 466/2012 of the National Health Council, which regulates research with human beings in Brazilian territory. The primary caregivers of the participating newborns signed the Informed Consent Form in duplicate.
RESULTS
Between 2022 and 2023, 291 premature newborns were registered in the NICU, of which 74 developed some type of skin lesion, totaling 112 lesions, distributed across various parts of the body, such as the head, neck, trunk, upper and lower limbs. Of the 112 lesions, 29.46% (n=33) were caused by medical devices, and in 11.60% (n=13) of cases, it was not possible to determine the origin of the lesions.
The medical devices used in this unit included: Peripheral Venous Access (PVA), nasal prongs, chest drain, polyurethane dressing, needles and catheters (for punctures), phototherapy device (causing burns), oximeter, and body hygiene wipes/towels for head support. Skin lesions not caused by medical devices included surgical wounds, injuries or trauma occurring during childbirth, congenital malformations, and diaper friction lesions. Table 1 presents the relationship between the use of medical devices and the location of lesions in hospitalized newborns. It was found that 100% of the lesions developed in the cervical region (n=2) and nasal septum (n=12) were caused by medical devices, with burns from phototherapy and polyurethane dressing changes causing lesions in the cervical region, and nasal prongs causing lesions in the nasal septum. In the head region, specifically in the occipital region, 77.8% (n=7) of the lesions were caused by medical devices, due to prolonged contact with the head support (disposable wipes/towels).
Table 1 - Relationship between the use of medical devices and the location of lesions in newborns hospitalized in the neonatal ICU
|
Location of the injury |
Medical device |
Total |
p-value |
||||
|
No |
Yes |
||||||
|
n |
% |
N |
% |
n |
% |
||
|
Cervical |
0 |
0 |
2 |
100 |
2 |
100 |
Χ2*=65,4 p<0,001 |
|
Face |
1 |
50 |
1 |
50 |
2 |
100 |
|
|
Nasal septum |
0 |
0 |
12 |
100 |
12 |
100 |
|
|
Occipital |
2 |
22,2 |
7 |
77,8 |
9 |
100 |
|
|
MMSS** |
2 |
28,6 |
5 |
71,4 |
7 |
100 |
|
|
MMII*** |
5 |
55,6 |
4 |
44,4 |
9 |
100 |
|
|
Thorax-Abdomen |
15 |
88,2 |
2 |
11,8 |
17 |
100 |
|
|
Perianal |
35 |
100 |
0 |
0 |
35 |
100 |
|
|
Others |
6 |
100 |
0 |
0 |
6 |
100 |
|
* Chi-square test (χ²), **Upper limbs, ***Lower limbs.
It was found that upper limb injuries were more frequent in newborns who used medical devices (71.4%, n=5) compared to those who did not (28.6%, n=2); these injuries were mainly caused by IV access, punctures, and polyurethane dressings. In the lower limbs, most injuries were not related to the use of devices (55.6%, n=5), however, 44.4% (n=4) were caused by their use (Table 1), such as oximeters, needles, or catheters for punctures and IV access.
Also in Table 1, it was found that most injuries in the chest and abdomen (88.2%, n=15) occurred in newborns who did not use medical devices; in this case, these injuries characterize surgical wounds resulting from surgical procedures. However, 11.8% (n=2) of the injuries were associated with the use of medical devices, such as chest drains and burns caused by phototherapy. Regarding lesions in the perianal region (100%, n=35), these were not caused by medical devices, but by friction resulting from diaper use.
Statistical analysis was conducted using the chi-square test (Χ²), which showed a significant value (Χ²=65.4, p<0.001), indicating a relevant association between the use of medical devices and the location of lesions in newborns hospitalized in the NICU.
Table 2 shows the relationship between the use of medical devices and the characteristics of the newborns. Newborns with a gestational age of less than 28 weeks presented the highest percentage of medical device use associated with lesions (68.8%, n=11, p<0.001); newborns between 28-31 weeks also showed a high rate of lesions related to the use of medical devices (69.2%, n=9, p<0.001). Newborns with a gestational age greater than 32 weeks showed a lower incidence.
Newborns weighing ≤1,000g and between 1,001-1,500g at birth presented high rates of injuries associated with medical devices, with 57.1% (n=8) and 55.0% (n=11), respectively. In contrast, neonates weighing between 1,501-2,500g presented a lower rate of injuries (11.8%, n=4), while those weighing ≥2,501g had an intermediate rate (32.3%, n=10). The differences were statistically significant (p<0.002), demonstrating a strong association between birth weight and the risk of injuries caused by medical devices (Table 2).
Table 2 - Relationship between the use of medical devices and the characteristics of newborns with skin lesions hospitalized in the NICU
|
Variable |
Medical device |
Total |
p-value |
||||
|
No |
Yes |
||||||
|
n |
% |
n |
% |
n |
% |
|
|
|
Gestational age |
|
|
|
|
|
|
Χ2*=23,5 p<0,001 |
|
< 28 weeks |
5 |
31,3 |
11 |
68,8 |
16 |
100 |
|
|
28-31 weeks |
4 |
30,8 |
9 |
69,2 |
13 |
100 |
|
|
32-33 weeks |
20 |
80,0 |
5 |
20,0 |
25 |
100 |
|
|
34-36 weeks |
15 |
83,3 |
3 |
16,7 |
18 |
100 |
|
|
≥37 weeks |
22 |
81,5 |
5 |
18,5 |
27 |
100 |
|
|
Birth weight |
|
|
|
|
|
|
Χ2=14,9 p<0,002 |
|
≤1.000g |
6 |
42,9 |
8 |
57,1 |
14 |
100 |
|
|
1.001 – 1.500g |
9 |
45,0 |
11 |
55,0 |
20 |
100 |
|
|
1.501 – 2.500g |
30 |
88,2 |
4 |
11,8 |
34 |
100 |
|
|
≥ 2.501g |
21 |
67,6 |
10 |
32,3 |
31 |
100 |
|
|
Length of hospital stay |
|
|
|
|
|
|
Χ2=13,5 p<0,004 |
|
Up to 7 days |
2 |
66,7 |
1 |
33,3 |
3 |
100 |
|
|
8 to 14 days |
10 |
90,9 |
1 |
9,1 |
11 |
100 |
|
|
15 to 30 days |
25 |
86,2 |
4 |
13,8 |
29 |
100 |
|
|
More than 30 days |
29 |
51,8 |
27 |
48,2 |
56 |
100 |
|
*Chi-square test (χ²)
Regarding the length of hospital stay, Table 2 shows that newborns hospitalized for up to 7 days presented 33.3% (n=1, p<0.004) of injuries caused by medical devices, while those hospitalized for 8 to 14 days had 9.1% (n=1, p<0.004) and, from 15 to 30 days, 13.8% (n=4, p<0.004). For newborns with prolonged hospital stays (more than 30 days), the rate of injuries associated with the use of medical devices increased, reaching 48.2% (n=27, p<0.004). All these injuries can be attributed to lack of repositioning, with most cases occurring in newborns with a gestational age greater than 32 weeks.
Table 3 presents the average characteristics of newborns with injuries caused by medical devices. Newborns with chest/abdominal injuries had higher birth weights (2,213g) compared to those with head/neck (1,707g) and limb (1,728g) injuries, with a nearly significant difference (p=0.054). The mean gestational age was also higher in the chest/abdomen group (33.9 weeks) compared to the head/neck and limb groups (both 31.2 weeks), indicating a trend without statistical significance (p=0.081).
Regarding Apgar scores, newborns with chest/abdomen injuries showed a slightly higher mean at both the 1st minute (5.32) and the 5th minute (7.63) compared to other regions, although these differences were also not statistically significant (p=0.284 and p=0.642, respectively) (Table 3).
Still in Table 3, the mean ECPRN score was higher in newborns with chest/abdomen injuries (5.95) compared to other regions, but without significance (p=0.077). The mean NIPS score was similar in all regions, with no significant difference (p=0.954). The mean healing time was longer in the chest/abdomen (19.9 days) compared to the head/neck (10.9 days) and limbs (8.88 days), with p=0.005, indicating significance. The mean hospitalization time was longer in head/neck injuries (50.1 days) compared to other regions, but without a significant difference (p=0.340).
Table 3 - Mean characteristics of newborns with injuries caused by medical devices hospitalized in the NICU
|
Characteristics |
Injuries caused by medical devices |
p-valor |
||
|
Head/neck |
Member |
Tórax/Abdome |
||
|
Average (DP*) |
Average (DP) |
Average (DP) |
||
|
Birth weight (g) |
1.707 (797) |
1.728 (873) |
2.213 (793) |
0,054 |
|
Gestational age |
31,2 (4,02) |
31,2 (7,78) |
33,9 (3,75) |
0,081 |
|
Apgar 1st minute |
4,72 (2,67) |
4,14 (2,57) |
5,32 (3,16) |
0,284 |
|
Apgar 5th minute |
7,24 (1,53) |
7,00 (91,9) |
7,63 (3,88) |
0, 642 |
|
ECPRN** |
5,52 (0,74) |
5,48 (0,60) |
5,95 (0,78) |
0,077 |
|
NIPS*** |
1,72 (1,91) |
1,71 (2,10) |
1,84 (2,01) |
0,954 |
|
Healing time |
10,9 (12,9) |
8,88 (7,19) |
19,9 (14,7) |
0,005 |
|
Length of Hospital Stay |
50,1 (30,3) |
43,7 (40,1) |
41,2 (17,2) |
0,340 |
* Standard deviation; **Newborn Skin Condition Scale; ***Neonatal Infant Pain Scale
Regarding the different treatments and interventions performed to treat or cure injuries caused by medical devices, it is noteworthy that all injuries underwent at least one type of treatment. Of the cases, 24.2% received two types of treatment, 9.1% were treated with three types, and 3.0% with four distinct interventions. The average healing time for the injuries was 12 days, while the average hospitalization time for these newborns was 56 days, with three deaths recorded.
Among the treatments and interventions performed, the use of laser stands out in 28.21% of cases (n=11), polyurethane sheet in 23.08% (n=9), Hirudoid® in 15.3% (n=6), and essential fatty acids (EFAs) also in 15.3% (n=6). To a lesser extent, other therapeutic approaches were employed, such as wound healing powder, dressings, silver alginate fiber, polyhexamethylene biguanide (PHMB), and adjustments in the neonate's positioning.
Figure 1, from the Multiple Correspondence Analysis (MCA), shows four main quadrants that group clinical variables and the location of injuries caused by medical devices in newborns. In the lower right quadrant, it is observed that chest/abdominal injuries are associated with a gestational age of 34-36 weeks, male sex, and hospitalization of 15-30 days.
Figure 1 - Multiple Correspondence Analysis (MCA) of clinical variables and location of injuries caused by medical devices in newborns
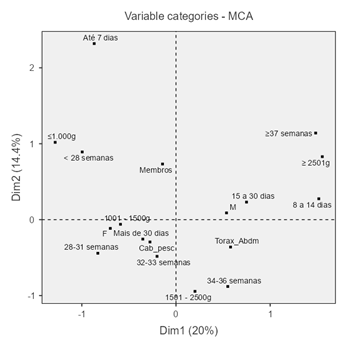
On the other hand, head and neck injuries were associated with a gestational age of 28-33 weeks, weight of 1,001-1,500g, female sex, and hospitalization exceeding 30 days, as indicated in the lower left quadrant. These data reinforce that neonates with lower weight and gestational age are more vulnerable, requiring prolonged hospitalizations. In Figure 1, in the upper left quadrant, it can be observed that injuries to the upper and lower limbs are related to low weight (≤1,000g) and gestational age less than 28 weeks.
DISCUSSION
Many premature newborns require essential hospital medical devices to maintain life, but these devices can cause iatrogenic injuries that compromise health and increase morbidity and mortality. A study in Brazil indicated that 31.34% of skin damage in neonates was caused by medical devices,(2) associated with prolonged pressure, poor positioning, or improper use. Another study, with 8,126 neonates from 22 hospitals in China, showed that 6.41% presented iatrogenic skin lesions, with 48% due to diaper dermatitis, 15% due to medical devices, 13% due to adhesives, and 13% due to physicochemical factors.(3)
A study conducted in a NICU in Iran reported that, among 368 hospitalized neonates, 126 presented skin lesions, with 12% of these associated with the use of nasal CPAP (Continuous Positive Airway Pressure). The authors highlight that, in hospital settings, especially in intensive care units, the use of technologies such as nasal CPAP, electrodes, sensors, adhesives, probes, and pulse oximeters significantly contributes to the development of pressure injuries (PIs). They also emphasize that prematurity exacerbates this risk due to reduced skin sensitivity, deficient blood perfusion, compromised tissue tolerance, malnutrition, and the presence of edema. (13)
In this research, newborns with hospital stays longer than 15 days showed a higher incidence of injuries associated with the use of medical devices. 112 injuries were recorded, with 29.46% attributed to these devices and 100% of nasal septum injuries related to them. These findings corroborate other authors.(14) who identified gestational age less than 28 weeks, weight below 1,000g, and the need for support devices, in addition to prolonged hospitalization, as the main factors.
A study in China revealed that for every 500g reduction in birth weight of a premature newborn, the risk of nasal septum injury can increase up to six times.(15) In southern Brazil, 19% of neonates in a NICU undergoing Non-Invasive Ventilation (NIV) presented with nasal septum injury, with gestational age between 30 and 35 weeks, weight less than 1,000g and, in most cases, lesions classified as stage I. Treatment included rotation of nasal prongs, application of Askina spray, hydrocolloid and Dersani combined with hydrogel, with recovery in up to seven days.(16) The use of hydrocolloid was highlighted as effective, and in the present study, polyurethane plates were used in 23% of cases, corroborating these practices.
The main mechanism responsible for the development of nasal septum injuries is inadequate or excessively tight fixation of the mask or prongs, usually to compensate for air leakage around the nose. To reduce the risk of these injuries, studies have highlighted the importance of training and raising awareness among NICU teams, prior organization of equipment and accessories, and the adoption of evidence-based protocols to minimize the risks of trauma.(14,16)
In addition to the need for medical devices, it is noteworthy that very low birth weight newborns (<1,500g) are indicated for the adoption of Minimal Handling. This practice, standardized by the multidisciplinary NICU team, seeks to reduce stress, pain, and the risks of intracranial hemorrhage caused by excessive handling. Thus, careful planning of therapeutic measures, essential to avoid the adverse effects of excessive manipulation, can ultimately contribute to the development of skin lesions.(17)
In this study, injuries in the head and neck region were associated with the use of towels or support scarves, resulting in contact and pressure damage. A study in Brasília highlighted inadequate positioning and lack of decubitus change as the main causes. (18) Prolonged use of these devices, combined with prematurity and low birth weight, increases the risk of serious injuries, as the thin stratum corneum and immature sebaceous and sweat glands do not provide sufficient moisture to protect the skin from retained heat.(4,6)
Researchers reported that approximately 31% of injuries in patients admitted to a maternal and child hospital in Pernambuco were located in the trunk region (umbilical, abdomen and thorax), a higher proportion than observed in other studies. The authors highlight that injuries to the thorax and abdomen are frequently associated with the use of catheters, gastric tubes, permanent needles and abdominal drains, and that, specifically in the thorax, the main causes include electrodes and trauma resulting from the use of adhesive tapes for fixing dressings and devices. In addition, 24% of injuries occurred in the upper and lower limbs.(19)
A study (20) analyzed 501 hospitalized neonates in three health units in Australia and New Zealand, finding that 41.4% presented injuries, located mainly on the feet (16.4%), cheeks (12.5%) and nose (11.3%), with 61.4% associated with medical devices. The main predictors were gestational age less than 30 weeks and hospitalization longer than 39 days, which was also reported by another study.(21) Our findings corroborate these results, showing a higher incidence of injuries in newborns with gestational age below 31 weeks, weight ≤1,000g and hospitalization longer than 30 days, in addition to similar locations.
Although medical devices are indispensable to the survival of premature infants, it is crucial that the multidisciplinary team acts carefully to minimize trauma, improper handling and damage caused by the medical devices used. (3)
A study conducted in a popular hospital in China evaluated 87 neonates with iatrogenic injuries admitted to the Neonatology department. The identified causes included removal of adhesive dressings (41.38%), skin scratches during blue light phototherapy (25.29%), diaper dermatitis (20.69%), and pressure sores associated with the use of ventilators and nasal CPAP (12.64%). The authors reported that length of stay, use of orotracheal intubation, and gastric tubes were risk factors for these injuries.(22)
To reduce skin injuries related to medical adhesives, it is essential to train healthcare professionals in the correct use of protective barriers and silicone-based removers. The skin should be clean, dry, and prepared before application, with adhesives carefully positioned to avoid excessive tension or pressure. Removal should be slow, using specific removers, and areas with adhesives should be monitored regularly to identify early signs of irritation or lesions.(23)
In this study, the most commonly used methods to treat injuries caused by devices were laser (28.21%) and polyurethane sheets (23.08%). Treatment also included careful cleaning and handling to prevent infections and promote healing. Recommended dressings include gauze, transparent film, hydrocolloids, polyurethane foams, alginates, and activated charcoal with silver, avoiding fully occlusive dressings and prioritizing those appropriate to the type and degree of injury.(24)
Furthermore, it is essential to emphasize the importance of training the nursing staff in the prevention and treatment of injuries in newborns. Regular training and evidence-based updates allow for the adoption of safe practices, reducing the risks associated with medical devices and promoting humanized care. A study in India used Plan–Do–Study–Act (PDSA) cycles, with interventions such as skin risk stratification, regular skin assessments, and protocol reinforcement. The injury rate dropped from 30 events per 1,000 applications to zero in five months, highlighting the effectiveness of evidence-based practices in reducing iatrogenic skin injuries in premature neonates.(25)
CONCLUSIONS
This study aimed to analyze skin injuries in critically ill newborns associated with the use of medical devices and to describe the treatments employed. The results showed a significant prevalence of injuries, especially in neonates with longer hospital stays, birth weight less than 1,000g, and gestational age below 31 weeks. The most frequent injuries occurred in the nasal septum and occipital region, with prolonged nasal prong pressure and inappropriate use of support materials being the main causes.
The main contribution of this study lies in expanding knowledge about the associations between clinical characteristics of newborns and the occurrence of injuries caused by medical devices, as well as offering evidence on effective treatments, such as the use of polyurethane sheets and laser therapy. The multifactorial approach to the data reinforces the importance of evidence-based clinical practices for the prevention and management of these injuries.
However, the study has limitations, such as being conducted in a single university hospital, restricting the generalizability of the findings. Furthermore, the analysis focused on specific devices, which may underestimate the occurrence of other types of injuries in critically ill neonates.
This study emphasizes the need for continuous training of multidisciplinary teams, prioritizing the appropriate selection of materials and the adoption of preventive protocols. Such strategies can minimize the incidence of injuries and improve clinical outcomes.
It is suggested that future research explore the effectiveness of new materials and technologies, as well as large-scale educational interventions, evaluating their influence on injury prevention. Furthermore, multicenter studies can offer a broader perspective, considering regional and institutional variations. Thus, it is expected that these investigations will contribute to advances in neonatal care, promoting the safety and well-being of hospitalized newborns.
REFERENCES
1. Silva RMM, Casacio GDM, Zilly A, Viera CS, Neves ET, Melo EMOP, Mello DF. Premature Newborns with the Potential to Develop Special Health Needs: An Approach by Triangulation of Methods. Aquichan. 2024;24(2):e2426. Doi: https://doi.org/10.5294/aqui.2024.24.2.6
2. Araújo DADS, Araújo JNDM, Silva ABD, Lopes JV, Dantas AC, Martins QCS. Alteration of skin condition in newborns admitted to neonatal intensive care: a concept analysis. Rev Bras Enfermagem. 2022;75,e20210473. Doi: https://doi.org/10.1590/0034-7167-2021-0473
3. Nie AM, Johnson D, Reed RC. Neonatal Skin Structure: Pressure Injury Staging Challenges. Advances in skin wound care. 2022;35(3):149–54. Doi: https://doi.org/10.1097/01.asw.0000818580.47852.68
4. Tenfen C, Barreto GMS, Moreira NM, Ferreira H, Zilly A, Silva RMM. Lesão de pele em recém-nascidos hospitalizados em terapia intensiva neonatal: estudo seccional. Rev Esc Enferm USP. 2024;58. Doi: https://doi.org/10.1590/1980-220X-REEUSP-2024-0058pt
5. Jani P, Mishra U, Buchmayer J, Maheshwari R, D’Çruz D, Walker K, et al. Global variation in skin injures and skincare practices in extremely preterm infants. World J Pediatr. 2023;19(2):139–57. Doi: https://doi.org/10.1007/s12519-022-00625-2
6. Zores C, Touzet M, Girard L, Caeymaex L, Kuhn P, Berne‐Audeoud F, et al. Recommendations on supporting neonatology healthcare givers from the French National Society. Acta Paediatrica. 2024. Doi: https://doi.org/10.1111/apa.17557
7. Giuffrida R, Borgia F, de Pasquale L, Guarneri F, Cacace C, Cannavò SP. Skin lesions in preterm and term newborns from Southern Italy and their relationship to neonatal, parental and pregnancy-related variables. G Ital Dermatol Venereol. 2018;154(4):400-04. Doi: https://doi.org/10.23736/s0392-0488.18.06068-6
8. Mallick AN, Bhandari M, Basumatary B, Gupta S, Arora K, Sahani AK. Risk factors for developing pressure ulcers in neonates and novel ideas for developing neonatal antipressure ulcers solutions. J Clin Neonatol. 2023;12:27‑33. Doi: https://doi.org/10.4103/jcn.jcn_84_22
9. Silva JC, Carvalho ESS, Sales IPPM, Blanes L, Camargo CL, Silva CTS. Evidence for the Treatment of Wounds in Newborns: An Integrative Review. Enfermería: Cuidados Humanizados. 2024:13(1). Doi: https://doi.org/10.22235/ech.v13i1.3220
10. Rocha ABO, Frutuoso DS, Souza TJ, Oliveira DF, Silva JN, Silva AF. Conhecimento da enfermagem na prevenção de lesões em prematuros. Rev Recien. 2022;12(37):34-44. Doi: https://doi.org/10.24276/rrecien2022.12.37.34-44
11. Olsson E, Ahl H, Bengtsson K, Vejayaram DN, Norman E, Bruschettini M, et al. The use and reporting of neonatal pain scales: a systematic review of randomized trials. Pain. 2021;162(2):353–60. Doi: https://doi.org/10.1097/j.pain.0000000000002046
12. Ji F, Li D, Lyu T, Yang T, Yuan H, Huang X, et al. (2024). Iatrogenic skin injuries in infants admitted to neonatal intensive care units: An investigation in 22 Chinese units. J Tissue Viability. 2024;33(2):197-201. Doi: https://doi.org/10.1016/j.jtv.2024.03.007
13. Abkenar MJ, Mojen LK, Shakeri F, Varzeshnejad M. Skin Injuries and its Related Factors in the Neonatal Intensive Care Unit. Iranian J Neonatol. 2020;11(4):94-98. Doi: https://doi.org/10.22038/ijn.2020.45342.1756
14. Biazus GF, kaminski DM, Silveira RDC, Procianoy RS. Incidence of nasal pressure injury in preterm infants on nasal mask noninvasive ventilation. Rev Paul Pediatria. 2023;41:e2022093. Doi: https://doi.org/10.1590/1984-0462/2023/41/2022093
15. Fu Y, Li X, Yu Y, Li R, Shi T. Summary of the best evidence for the prevention of nasal injury in preterm infants with nasal noninvasive ventilation. Translational Pediatrics. 2024;13(2):224. Doi: https://doi.org/10.21037/tp-23-465
16. Grebinski ATKG, Silva CC, Tonial DA, Zilly A, Silva RMM. Nasal septal injury in hospitalized newborns: exploratory descriptive study. Online Braz J Nurs. 2023;22:e20236630. Doi: https://doi.org/10.17665/1676-4285.20236630
17. Martins KP. Protocolo de manuseio mínimo para recém-nascidos prematuros em unidade de terapia intensiva neonatal [Dissertação]. [Curitiba]: Universidade Federal do Paraná; 2020. 188p.
18. Faria TF, Kamada I. Úlceras por pressão em neonatos internados em uma Unidade de Terapia Intensiva Neonatal: Série de Casos. Estima–Brazilian J Enterostomal Therapy. 2017;15(2):115-19. Doi: https://doi.org/10.5327/Z1806-3144201700020008
19. Ferreira DLS, Fernandes FECV, Melo RA, Aguirre, VCSP, Mola R. Profile of patients with skin lesions in a maternal and child hospital. Braz J Health Review. 2022;5(2):5562–76. Doi: https://doi.org/10.34119/bjhrv5n2-136
20. August DL, Kandasamy Y, Ray R, Lindsay D, New K. Fresh Perspectives on Hospital-Acquired Neonatal Skin Injury Period Prevalence From a Multicenter Study: Length of Stay, Acuity, and Incomplete Course of Antenatal Steroids. J perinatal neonatal nursing. 2021;35(3):275–83. Doi: https://doi.org/10.1097/jpn.0000000000000513
21. Broom M, Dunk AM, E Mohamed AL. Predicting Neonatal Skin Injury: The First Step to Reducing Skin Injuries in Neonates. Health Services Insights. 2019;12:1-10. Doi: https://doi.org/10.1177/1178632919845630
22. Deng H, Li C, Yu N. Factors Influencing Iatrogenic Skin Injury in Neonates and Nursing Strategies. Alternative therapies in health and medicine [Internet]. 2024;30(11):185–89. Disponível em: https://pubmed.ncbi.nlm.nih.gov/38687850/
23. Downie F, Allaway R. Preventing Medical Adhesive Related Skin Injury (MARSI): introducing a skincare regimen for good practice. Wounds [Internet]. 2024;20(1):38. Disponível em: https://wounds-uk.com/wp-content/uploads/2024/02/WUK_20-1_MeetingReport-MARSI-v2-web.pdf
24. Steen EH, Wang X, Boochoon KS, Ewing DC, Strang HE, Kaul A, et al. Wound Healing and Wound Care in Neonates: Current Therapies and Novel Options. Advances in skin wound care. 2020;33(6):294–300. Disponível em: https://alternative-therapies.com/oa/pdf/10040.pdf
25. Kar S, Jarain VZL, Karmakar S, Devi U, Som TK, Mohanty PK, et al. Quality improvement initiative to reduce Medical Adhesive Related Skin injury (MARSI) in very preterm babies admitted to neonatal intensive care unit. BMJ open quality. 2024;13(Suppl 1):e002697. Doi: https://doi.org/10.1136/bmjoq-2023-002697
Funding and Acknowledgments:
This study was supported by the State University of Western Paraná (UNIOESTE), Brazil; and the University Hospital of Western Paraná (HUOP), Brazil.
Conflict of Interest Statement
“Nothing to declare”.
Authorship Criteria (Author Contributions)
Carolina Tenfen: Study conception and planning; data acquisition, analysis, and interpretation; writing and critical review; approval of the final version.
Ivaneliza Simionato de Assis: Study conception and planning; data acquisition, analysis, and interpretation; writing and critical review; approval of the final version.
Geisyelli Alderete: Data analysis and interpretation; writing and critical review.
Marcos Augusto Moraes Arcoverde: Data acquisition, analysis, and interpretation; writing and critical review.
Bruno Taiki Takahasi: Data analysis and interpretation; writing and critical review.
Maria Fernanda Munhak da Silva: Data analysis and interpretation; writing and critical review.
Rosane Meire Munhak da Silva: Study conception and planning; data acquisition, analysis, and interpretation; writing and critical review; approval of the final version.
Scientific Editor: Ítalo Arão Pereira Ribeiro. Orcid: https://orcid.org/0000-0003-0778-1447
Rev Enferm Atual In Derme 2026;100(1): e026023